Many women wonder what HSG and HSG are, how HSG and HSG of the fallopian tubes are done, how informative and safe this procedure is.
Hysterosalpingography and ultrasound hysterosalpingoscopy are quite often used in gynecological practice. They allow you to safely check the patency and presence of deformations of the internal female genital organs, as well as detect morphological pathology. These procedures are highly informative and have a low incidence of side effects.
Hysterosalpingography (HSG)
What is hysterosalpingography? HSG is a research method that allows you to carefully examine the inner surface of the uterus and fallopian tubes. It provides maximum information for congenital or acquired diseases that are accompanied by changes in the structure of these organs. To do this, a series of x-ray images are taken.
HSG is prescribed if the following diseases and pathologies are suspected:
- congenital anomalies of the development of the internal female genital organs;
- obstruction of tubal patency after inflammatory processes or an abortion;
- benign and malignant neoplasms;
- to diagnose tubal infertility in a patient after excluding hormonal causes (including before IVF);
- specific inflammatory processes (tuberculosis, syphilis);
- isthmic-cervical insufficiency;
- a history of ectopic pregnancies;
- spontaneous abortion at any stage of pregnancy;
- pathologies of previous births.
Typically, HSG x-ray or hysteroscopy is performed on patients who have already undergone a complex of preliminary examinations (CBC, OAM, biochemical blood parameters, ultrasound of the pelvic cavity).
Contraindications for the test
HSG during pregnancy in gynecology is strictly prohibited. There is strong evidence negative influence contrast, as well as X-ray radiation to the fetus. Therefore, the only approved method for diagnosing pathology during this physiological state remains a standard ultrasound of the fallopian tubes. Also, HSG cannot be performed during lactation.
Also, an absolute contraindication to the study is the presence of any allergic reaction to drugs used as contrast. Many guidelines also strongly recommend performing a hypersensitivity test before initiating HSG.
Conducting research is also prohibited under a number of conditions:
- inflammatory processes in the patient’s genital organs;
- the presence of functional kidney or liver failure;
- decompensated cardiovascular diseases (coronary disease, congenital defects);
- any form of uterine bleeding;
- hormonal imbalances associated with diseases thyroid gland;
- increased tendency to form blood clots (thrombophilia, thrombophlebitis).
Relative contraindications to tubal HSG include inflammatory changes in general analyzes blood (leukocytosis, increased BSR, increased number of neutrophils) and urine, bacteriological examination of a vaginal smear.
Ultrasound hysterosalpingoscopy (USGSS)
Ultrasound hysterosalpingoscopy is actually a transvaginal ultrasound examination of the pelvic organs with the introduction of glucose, furatsilin or saline solution into the lumen of the uterus. Ultrasound hysteroscopy provides a dynamic image of the distribution of fluid in the uterine cavity and fallopian tubes.
This method has a number of advantages over GHA. Ultrasound hysterosalpingoscopy does not require the administration of contrast, which eliminates the possibility of allergic reactions and also reduces the list of contraindications. Also, this method does not expose the patient’s body to x-ray radiation. With ECHO HSG of the fallopian tubes, complaints of pain and a feeling of heaviness are less common.
Ultrasound hysterosalpingography for this large quantities advantages, also has its disadvantages. It visualizes the organ cavity worse, which reduces the informativeness of the diagnosis. The quality of the results depends on the qualifications of the diagnostician, which, if there are errors, has negative consequences in the future.
Preparing for the study
Many patients are concerned about the question of how to prepare for HSG and USGSS so that the results of the study are as informative as possible. After prescribing the procedure, the attending physician carefully informs all of them about this.

Contrasting the uterus and fallopian tubes
Preparation for tubal HSG and hysterosalpingoscopy consists of several important steps. First, the gynecologist needs to conduct a general examination of the condition of the main functional systems body. Additionally, the patient is tested for some common infectious diseases (AIDS, syphilis, gonorrhea). In the evening the day before the test, it is also recommended to perform a cleansing enema to remove feces from the intestines.
The study is carried out on days 5-10 of the menstrual cycle. This allows, on the one hand, to almost completely eliminate pregnancy in the patient, and on the other, a thinner endometrium contributes to less intensity of discomfort during the procedure and better visualization of organs.
On the day of an HSG or ultrasound to determine the patency of the fallopian tubes, it is necessary to thoroughly clean the patient’s external genitalia, as well as shave the pubic hair, as it may interfere with the examination.
The HSG procedure in gynecology involves the patient emptying her bladder immediately before the start of the study. It is also necessary to remove all metal jewelry and items of clothing in the genital and pelvic area. Hysteroscopy, on the contrary, requires that the patient have a full bladder before the examination.
Research methodology
X-ray examination of pipes for patency is carried out in a special room. The patient takes a place on a standard table for gynecological interventions. Both HSG and ultrasound examination of the patency of the fallopian tubes begin with an external examination by a specialist of the woman’s external genitalia, vagina and cervix using a gynecological speculum. After this, an antiseptic treatment is carried out and a catheter is inserted into the cervical canal, through which a contrast agent is injected.

Introduction of saline solution into the uterine cavity and USGSS
The first image is taken after the injection of 2-3 ml of contrast. After a short period of time, a second portion of the substance is supplied, which facilitates its penetration into the lumen of the fallopian tubes. It is at this moment that the second photo is taken. With normal tubal patency, some contrast material enters the abdominal cavity. If necessary, a third picture is taken after 20-30 minutes.
Use of medications during the procedure
HSG is considered an almost painless procedure, as is ultrasound hysterosalpingoscopy. Therefore, anesthesia is used only for severe pain in a very small proportion of patients.
In some clinics, before the study, antispasmodics (drotaverine, papaverine) are additionally administered, which allows you to relax the cervix and avoid problems with inserting a catheter into the uterine cavity.
Side effects during HSG
Checking the patency of the fallopian tubes using contrast injection may be accompanied by the development side effects, although in general the procedure is considered absolutely safe. About a third of patients note discomfort in the abdominal area, which sometimes turns into nagging or aching pain.
The most dangerous complication of the procedure is the development of local and general allergic reactions of varying severity. Cases of anaphylactic shock with systemic hemodynamic disturbances have been described. Therefore, medical personnel approach this procedure with special attention and caution.
If the research methodology is violated, traumatic damage to the uterine mucosa by the catheter is possible, which is clinically manifested by bleeding from the vagina.
Research results
Hysteroscopy allows for a thorough examination of the uterine cavity and fallopian (uterine) tubes. The radiologist obtains high-quality images of the anatomical structure of the patient’s internal genital organs. They can be used to visualize signs of congenital malformations, the consequences of inflammatory processes, and the presence of tumors. Hysterosalpingography cannot determine the type of oncological process; therefore, if it is detected, a biopsy with cytological examination is usually performed. Ultrasound hysterosalpingoscopy also provides information about the condition of the uterine walls and the presence of pathology in the myometrium.
Hysterosalpingography remains the leading and simple method diagnosing the causes of tubal infertility and anomalies in the development of the internal genital organs in women. Along with it, ultrasound hysteroscopy is performed, which is characterized by less information content and greater subjectivity of the results, but has fewer contraindications.
A transcript of the results is usually sent to the attending gynecologist or given to the patient immediately after the study. They not only help to assess the patency of the fallopian tubes using ultrasound, but also determine further tactics for diagnosing and treating the patient.
One common cause of infertility is obstruction of the fallopian tubes. There are several ways to diagnose this condition. However, the most used of them is the consequences of which are not very pleasant, but quite tolerable.
This study can be carried out on different days of the menstrual cycle as prescribed by a doctor. You should not overeat the night before and eat and drink on the day of the examination. Before HSG, you need to do an enema, empty your bladder and shave your pubic hair.
HSG, the consequences of which can be minimized by undergoing necessary examination before it, it is usually performed without anesthesia, however, at the request of the patient, light anesthesia can be used. A week before the test, you need to take urine and blood tests, make vaginal smears and be tested for HIV, syphilis and hepatitis.
One of the most unpleasant, but possible consequences HSG is an inflammatory process. Therefore, after the procedure you need to pay close attention to your health. Fever, pain and after HSG for more than three days are a reason to consult a gynecologist.
The study cannot be carried out if there is an inflammatory process in the genital tract or if it has recently been suffered. Exacerbation of a general disease is a contraindication to the procedure (pyelonephritis, influenza, pneumonia).
X-ray contrast agent may cause allergies. Therefore, it is necessary to find out the reaction to the drug used; as a rule, it contains iodine.
In a cycle in which HSG is performed, the consequences of which can be pleasant, it is imperative to protect yourself, even if long time pregnancy did not occur. This is due to the fact that after the study the likelihood of its occurrence increases significantly due to the washing effect.
A contrast agent injected into the tubes eliminates small adhesions that previously interfered with conception. This is truly an established fact, which is why many women have high hopes for this procedure.
HSG, the results of which are of great value for identifying the causes of infertility, is performed in an X-ray room on a special chair. After a two-handed examination, several images are inserted into the uterus and taken.
This procedure is tolerated differently by patients. Some note only discomfort, others complain of severe pain. Most likely this is due to the sensitivity threshold, which is individual for each person.
After an HSG, there may be some slight bleeding, so you should take a sanitary pad with you. It usually goes away within a couple of hours.
After the examination, there are painful sensations reminiscent of the onset of menstruation. They are especially evident in sitting position. A slight rise in temperature and mild symptoms are also possible. These phenomena are normal in the first few days.
As a result of the HSG, the patient receives images in her hands, from which you can see whether they are passable and, if not, then in which part. In addition, they can be used to diagnose diseases such as endometriosis, tuberculosis of the reproductive system, various pathologies, including congenital ones (bicornuate, saddle-shaped).
It is important to remember that in 20% of cases, HSG gives a false diagnosis of tubal obstruction. This can happen if a woman has long and narrow hair. Then the contrast agent simply does not have time to get into the abdominal cavity.
In addition, due to stress and anxiety, spasm of the tubes may occur. Therefore, it is necessary to drink no-shpa before the study. To prevent the inflammatory process, the doctor may prescribe a course of suppositories, tampons or antibiotics.
Thus, HSG, the consequences of which can be both negative (inflammation) and positive (long-awaited pregnancy), is a very informative procedure. It allows you to check the patency of the fallopian tubes, detect their pathologies, as well as the uterus. To prevent negative consequences it is necessary to follow the recommendations of the gynecologist.
According to the standards of the World Health Organization, infertility in women or men is said if a couple has been sexually active for a year without resorting to contraception, but conception has not occurred. There can be many reasons for this. One of the most common is fallopian tube obstruction.
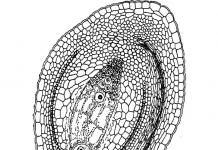
The fallopian tubes (or fallopian tubes) are narrow canals that connect the ovaries to the uterus. Their length is approximately 10 cm with a diameter of up to 1 cm. It is along them that the fertilized egg moves to the uterus. If her path is blocked, then a normal pregnancy will not be able to occur. With partial obstruction, a dangerous condition for the woman is likely to develop - an ectopic pregnancy.
HSG of the fallopian tubes is an effective study based on the analysis of the passage of X-rays or ultrasound waves through the tissue being studied after the administration of an iodine-containing contrast agent or other liquid (for ultrasound). Iodine-based preparations are considered the least toxic when exposed to ionizing radiation. In addition, sometimes patients can become pregnant immediately after HSG. Why is this happening? What is this procedure? And also how to prepare for it, how it goes, are there any contraindications and answers to other most important questions - in the proposed article.
What is HSG or hysterosalpingography? HSG in gynecology is medical examination, which allows you to check the fallopian tubes for patency and examine the uterine cavity.
There are two main forms of the procedure - x-ray and ultrasound hysterosalpingography (US-HSG). In the first case, a solution - glucose, furatsilin or physiological - is injected into the uterine cavity, in the second - Urotrast, Verografin or Urografin. It is noteworthy that earlier the study was carried out with Lugol's solution, but it caused irritation of internal tissues, so an alternative was subsequently found.
How to prepare for research
Preparation for HSG depends on whether the procedure will be performed using x-rays or ultrasound.
To obtain reliable results, a week before the appointed date, you cannot douche and use intravaginal intimate hygiene products - tampons, suppositories, tablets, local remedies for sexually transmitted and other diseases are prohibited.
1-2 days before the session it is better to abstain from sexual intercourse.
The patient should undergo a standard gynecological examination. If for some reason it is not possible to establish the fact of absence of pregnancy, blood is donated for hCG.
The evening before the examination, the woman should have an enema or take Fortrans.

On the day of the procedure, all hygiene procedures should be carried out, including hair removal.
The scan is done on an empty stomach. You are allowed to drink a glass of still water.
Before the x-ray, you must empty your bladder and remove all metal objects.
Preparation for ultrasound-type hysterosalpingography is the same, only the bladder should be as full as possible during the session.
Indications and contraindications
The main indication for fallopian tube HSG is the inability to conceive a child over a long period of time. In addition, if a woman has a history of miscarriages, the doctor will definitely refer her for the procedure.
- infertility of non-hormonal origin;
- physiological deviations in the structure of the organs of the reproductive system - acquired (for example, after injuries) or congenital;
- complicated course of previous pregnancies, difficult childbirth, ectopic implantation of the embryo, early or early miscarriages later in the anamnesis;
- isthmic-cervical insufficiency;
- suspicion of tuberculosis, fibroids, the presence of polyps, the need for differential diagnosis of the nature of the identified tumor;
- monitoring of complications of previously suffered or chronic diseases (endometriosis, salpingitis), postoperative observation.
Sometimes HSG performs a screening function, for example, when planning pregnancy, even in the absence of problems with conception. The procedure is a mandatory step in preparation for ovulation stimulation, which is contraindicated in case of tubal obstruction.
Hysterosalpingography may be prescribed in other cases at the discretion of the doctor, for example, if the patient has suspicious discharge.
In what cases should hysterosalpingography not be performed?
There are contraindications for fallopian tube HSG:
- inflammation of the uterus and its appendages;
- if the cleanliness of the vagina is rated below the second degree, which may indicate an inflammatory or infectious process;
- pregnancy, since X-rays may expose the fetus to radiation. To Echo-HSG this contraindication does not apply;
- suspected ectopic pregnancy;
- severe diseases of the cardiovascular system;
- allergy to the components of the contrast solution used during the procedure.
How to do an x-ray of the fallopian tubes
The HSG procedure, which includes x-rays of the uterus and both fallopian tubes, works as follows.
To eliminate the occurrence of pain, the patient is administered antispasmodic drugs half an hour before the procedure. They reduce the spasm of smooth muscles and are generally calming.
A special table will be equipped for the GHA. Various gynecological operations are usually performed on these patients. Preparatory procedures take longer than the examination itself, which lasts about 15-20 minutes (less often – up to 40 minutes).
The patient is positioned so that her pelvis is on the edge of the table. The legs are placed in a bent position on holders. The external genitalia are treated with an antiseptic solution.
Next, with the help of gynecological speculum, access to the cervix is gained. After this, a liquid with contrast is pumped through the vagina and cervix directly into the uterus and narrow tubes. To do this, the doctor uses a thin tube that is connected to a syringe. At the first stage, 2-3 ml is injected and an image is taken. To obtain a second radiograph, another 3-4 ml of solution is injected. If necessary, half an hour later the picture is recorded on the x-ray for the third time.

The basis of the injected solution is a contrast agent, for example, Ultravist, Verografin. Its key feature is the presence of iodine.
For ultrasound diagnosis of fallopian tube patency, a normal saline solution with a volume of 80-100 ml is used and the nature of the passage of the liquid substance is studied using the intravaginal ultrasound method.
Once the procedure is completed, the patient is placed on a bed where she should rest for about an hour.
What are the normal results of hysterosalpingography?
The doctor draws his conclusions based on the images obtained, providing the patient with a complete transcript of them. If everything is in order, then they will depict a uterus in the shape of a triangle, which has two fallopian tubes, which are thin branches. They open into the abdominal cavity, where the ovaries are located.
Spots may be visible on the x-ray. This is how the contrast agent appears, which was able to enter the uterine cavity and penetrate the fallopian tubes, and then exit into the abdominal cavity. This picture indicates absolute patency of the fallopian tubes.
If only one pipe is completely visible on the image, then only it is passable; if both are not fully visible, then they are diagnosed as completely obstructed. Usually the contrast stops at a certain area. In medical practice, there are cases of partial obstruction.
The accuracy of the result depends on the correct preparation of the patient and the choice of the day of examination, since HSG needs to be done in the first half of the menstrual cycle.
The study allows you to diagnose polyps, fibroids, hydrosalpinx, adhesions, including those pressing on the outside of the pipe.
Comparisons of methods
In addition to hysterosalpingography itself, there are other methods for checking the patency of the fallopian tubes. These include:
- laparoscopy. To conduct the study, specialists make a puncture in the abdominal wall and insert a device – a laparoscope – inside. It is equipped with a video camera and a small flashlight, which allow you to study the patient’s reproductive organs in detail. Often such a study is chosen when it is necessary to remove adhesions;
- blowing of the fallopian tubes. This method is used only if a woman is allergic to the contrast agent that is administered during HSG. To do this, using a rubber tube and pressure gauges, air is heated and forced inside.
MSG and GHA - what is the difference
The difference between hysterosalpingography and metrosalpingography is in the name. The fact is that the components of the terms “hystera” and “metra” essentially mean the same thing - “uterus”. Therefore, preparation for HSG, or MSG, of the fallopian tubes and the examination process are synonymous.
Which is better - ultrasound or x-ray
A procedure called hysterosalpingography can be performed in two forms - x-ray or ultrasound. Each of them has both advantages and disadvantages, so it is impossible to give a definite answer to the question. The decision to conduct one or another type of examination is made by the supervising physician based on the patient’s condition.
GHA or Echo-HSG
Let's take a closer look at the differences between X-ray and Echo-hysterosalpingography.
Unlike radiographic HSG, Echo HSG is an ultrasound scan. Thus, all examination results will be visible on the monitor directly during the procedure. Its main advantages are the absence of the slightest radiation and the need to be admitted to a hospital. The disadvantage is that the clinical picture can only be assessed by the sonologist performing the scan. X-ray images will be available to different specialists.
In order to perform an Echo-HSG, it is necessary to choose the right time. The ideal period is the beginning of ovulation, since the cervix is as relaxed as possible during these days of the cycle.
The algorithm for performing echohysterosalpingography does not differ from x-rays. The patient is also given a fluid that should travel through the fallopian tubes. The difference is that the solution is not administered in stages, but in one dose. In this case, a saline solution is used, not an iodine-containing dye. The volume of injected liquid is also much larger.
The decision to conduct an HSG or Echo-HSG is made by the doctor himself, after analyzing the patient’s medical record.
On what day of the menstrual cycle can hysterosalpingography be done?
If the doctor has prescribed an HSG with x-ray, then, as a rule, the examination is carried out in the first half of the menstrual cycle, namely from the sixth to the twelfth days, if we are talking about a standard thirty-day cycle. X-rays show the clearest images during ovulation, because during this period the endotherm is very thin.

Menstruation after HSG does not always come as usual; sometimes the cycle after HSG is disrupted.
Pregnancy after HSG
After HSG, pregnancy can occur already in the current menstrual cycle. However, doctors do not recommend starting conception in the same month if X-ray techniques were used. Affects the reproductive system ionizing radiation, which can adversely affect the development of the fetus or cause a miscarriage.
Probability of conception after HSG
Ultrasound HSG of the fallopian tubes is not only a check of the state of their patency, but also a medical therapeutic procedure. The pressure created by the liquid on the internal walls helps to break small adhesions, thereby eliminating the cause of obstruction. Therefore, it is after such a study that a woman can become pregnant. If pregnancy does not occur after HSG and obstruction is not confirmed, then the doctor will look for other causes of female infertility.
They write on the Internet that after HSG, women have an increased risk of ectopic pregnancy. However, this is just a myth, since the mentioned pathology is directly related to deviations in the structure and functionality of the fallopian tubes. They have nothing to do with diagnosis.
When can you plan a pregnancy after hysterosalpingography?
Pregnancy after HSG can be planned no earlier than six months later, because at the time of the procedure the patient’s body receives a large dose of radiation.
Ultrasound waves are harmless, therefore, after passing the Echo-HSG, the described restrictions are absent.
About the delay after the study
The procedure is still stressful for female body. Therefore, a delay after HSG of several days is considered normal. If the patient has had sexual intercourse, then it is worth checking whether the cycle failure is associated with pregnancy.
What complications are possible with hysterosalpingography?
HSG of the fallopian tubes is a completely safe procedure, and therefore most often does not cause negative consequences or complications.
In rare cases, pronounced allergic reactions to a contrast agent. Particular caution should be exercised by women with bronchial asthma and prone to allergies.
The carelessness of the doctor can lead to perforation of the uterus and damage to other tissues.
In patients with chronic infectious diseases exacerbation is possible, up to endometritis and inflammation of the appendages.
How will you feel after hysterosalpingography?
Many people write on the Internet: “Hysterosalpingography is very painful.” However, if the doctor performed all the manipulations correctly and the patient was prepared, then there will be no discomfort during the procedure.
After HSG, minor pain in the lower abdomen may appear. They are triggered by contractions of the uterus. This happens due to stress or is a reaction to the injection of a solution. To reduce discomfort, you can take a pain reliever.
For one to two days, the patient may be bothered by spotting. They represent remnants of the contrast agent and endometrial particles. It is recommended to use sanitary pads for some time after the procedure.
Hysterosalpingography is needed to identify pathologies of the fallopian tubes - the most common cause infertility. This study can tell a lot about the state of the reproductive organs and the reproductive system in general. It really helps a lot of women. As statistics show, pregnancy after HSG of the uterus and fallopian tubes occurs in the vast majority of patients - due to the therapeutic effect provided or prescribed based on the results of treatment.
HSG is a diagnostic procedure in which a contrast agent is injected into the uterus and fallopian tubes. After this, several x-rays are taken. HSG is the main method for diagnosing tubal obstruction. The study also helps to identify many pathologies of the uterus.
Indications
HSG is performed if the following diseases are suspected:
- uterine fibroids with submucosal nodes;
- hyperplastic processes of the endometrium;
- polyps;
- adenomyosis;
- tuberculosis;
- tubal factor infertility;
- isthmicocervical insufficiency.
Based on the purpose of use, HSG of the fallopian tubes and uterus can be performed on different days of the menstrual cycle.
If ICI or infertility caused by tubal obstruction is suspected, hysterosalpingography is done in the luteal phase. That is, in the second half of the menstrual cycle, shortly before the onset of menstrual bleeding.
If it is necessary to identify intrauterine pathological growths of the endometrium due to endometriosis, the study is scheduled for the 7th or 8th day of the cycle. If the presence of myomatous nodes in the uterus is suspected, HSG is performed on any day. But only in the absence of bleeding: menstrual or pathological.
Contraindications
HSG is not performed for some diseases. The reason for the impossibility of performing a diagnostic procedure can be both diseases of the genital organs and general somatic pathologies. Main contraindications:
- Any acute infectious processes. Including sore throat, flu, boils, etc.
- Severe diseases of internal organs: renal, liver failure.
- Hyperthyroidism. This is an increased function of the thyroid gland. The study is contraindicated because the injected contrast agent contains iodine.
- Intolerance to iodine preparations is an absolute contraindication to HSG.
- Active inflammation of the genital organs. This includes any acute or torpid processes of the uterus, fallopian tubes, vagina, etc.
Preparation for GHA
The woman undergoes examination before performing HSG. She undergoes general clinical tests and smears from the urogenital tract. If signs of inflammation are detected in the blood (leukocytosis, increased ESR), the procedure is not performed.
1 week before HSG, it is necessary to avoid the use of any vaginal suppositories or tablets. The exception is medications prescribed by a doctor specifically to prepare for the procedure. Half an hour before the HSG, in order to reduce discomfort, you can take an antispasmodic tablet (drotaverine).
Preparation for HSG in case of detection of inflammatory diseases
Sometimes a smear taken from the genital organs on the eve of an HSG shows the presence of an inflammatory process. The smear may contain:
- leukocytes;
- mucus;
- bacteria;
- mushrooms;
- Trichomonas.
All these changes are grounds for canceling the tubal examination procedure. Because with the introduction of a contrast agent, as well as due to contraction of the muscles of the reproductive organs, an upward spread of infection is possible. It can enter the fallopian tubes and even the abdominal cavity with the development of pelvioperitonitis.
Therefore, if inflammatory processes are detected, special preparation for HSG is required. Sanitation of the urogenital tract is necessary. It is carried out in various ways, depending on the identified violations of the biocenosis. The following may be detected:
- sexual infections;
- transient flora;
- candida;
- opportunistic bacteria in increased quantities.
If the cause of inflammatory changes in the smear is opportunistic or transient flora, local antiseptics are used. They are prescribed in the form of candles. Douching is also used. After the course of therapy you need to wait 2 weeks. Then - make a tank seeding. When the concentration of bacteria decreases below 10 to 4 degrees CFU, the procedure can be performed if the smear on the flora is normal and there are no inflammatory symptoms.

If sexually transmitted infections are detected, antibiotic therapy is required. In the case of gonorrhea, ceftriaxone is prescribed. For trichomoniasis, ornidazole is used. For chlamydia, doxycycline is used. In 2 weeks PCR method examine a smear from the urogenital tract. The absence of pathogenic microorganism DNA is considered a criterion for cure. In this case, HSG can be performed.
Sometimes Candida fungi are detected. They talk about candidiasis. The disease is popularly called thrush. To cure it, it is usually enough to take 1 tablet of fluconazole 150 mg. After this, after 2 weeks, a smear is taken for the flora. If pseudomycelium and budding cells are not detected, there are no inflammatory changes in the smear and there are no clinical signs of candidiasis, HSG is performed as soon as the favorable moment for this occurs (the necessary phase of the cycle).
How is tubal HSG performed?
The woman sits on a radiolucent gynecological chair. She is in position for vaginal surgery. The genitals are treated with antiseptics. A bimanual examination is performed. Speculums are then inserted into the vagina. The anterior lip of the cervix is grasped with forceps.
The contrast agent is injected using a cannula. This is a long tube that has a syringe attached to it. The doctor inserts the rubber tip of the tube into cervical canal. The external opening must be hermetically sealed. The doctor then removes the speculum. The woman is placed in the position necessary to take x-rays.
First, 3 ml of contrast is injected and an image is taken. Its goal is to obtain an image in which you can see the relief of the uterine cavity. Then another 3 ml of contrast is injected. The uterus fills more tightly. At this point the second shot is taken.
In most women, after the second injection of contrast, the fluid enters the fallopian tubes and then into the abdominal cavity. But if this does not happen, the doctor may inject more contrast material and then take a third photo to examine the condition of the fallopian tubes.
Tubal HSG results are normal
On normal radiographs, the uterine cavity has the shape of a triangle. It is directed upward with its base. Its width is about 4 cm. In the lower part, the uterus passes into the isthmus. Its length is from 8 to 10 mm. Next comes the cervical canal. Normally, it has the shape of a cone, cylinder, or can also be spindle-shaped, which depends on the phase of the menstrual cycle.
The X-ray shows the fallopian tubes as thin lines. They look like threads or ribbons. They usually have a sinuous shape. The interstitium is short and looks like a cone. After the narrowing comes the isthmic section - long and narrow. Then it turns into ampullary - it is wide and not always clearly visible in photographs.
Pathological changes
By performing an HSG of the fallopian tubes, it is possible to detect their obstruction. Most often it develops in the interstitial region. On the x-ray, the doctor sees that the contrast does not pass beyond a certain point. It can accumulate when it reaches an obstacle, stretching the pipe section. In this place, expansion is visualized in the form of an accumulation of contrast agent.
Other pathologies of the fallopian tubes that can be detected:
- tuberculosis - manifested in photographs by expansion of the interstitial part of the fallopian tube;
- salpingitis - the ampullary part of the tube has a uniform expansion in the form of a flask, which is associated with the accumulation of inflammatory exudate in it (it is mixed with contrast during the study);
- sactosalpinx - accumulation of fluid, occurs as if inflammatory diseases, and with tumor lesions of the tubes, as well as endometriosis.
Pathologies of the uterus are detected. Among them:

- malformations - incomplete septum, bicornuate uterus, infantile, saddle-shaped, double, unicornuate uterus;
- endometrial hyperplasia and the appearance of polyps (thanks to GHA, their number, size, location can be identified);
- cancer of the uterine body - an x-ray reveals deformation of the uterine cavity, filling defects with uneven contours.
When injected into the uterus, the contrast liquid spreads evenly over its surface. It helps to visualize all its irregularities. If filling defects appear, the doctor suspects polyps. When the contours of the uterus are uneven, hyperplastic processes occur.
However, with uterine pathology, differential diagnosis of various pathologies is difficult. Often formations of different origins look the same. For example, a polyp cannot be distinguished from a submucosal fibroid. Although, based on indirect evidence, assumptions can be made. Polyps are usually smaller than fibroids. They have clear contours and are not accompanied by an enlargement of the uterine cavity.
HSG helps the doctor in diagnosing endometriosis. In the picture, the doctor sees many contour shadows. Foci of endometrioid tissue can also be found in the fallopian tube.
HSG is one of the ways to detect isthmicocervical insufficiency. On an x-ray, you can determine the width of the isthmus (isthmus) in the second phase of the cycle. Normally it is no more than 4 mm. In the case of ICN, the width can increase to 1.5 cm or more.
Hysterosalpingography is a valuable tool in the diagnosis of diseases of the uterus and fallopian tubes. The technique is widely used in reproductive medicine. Thanks to HSG, it is possible to identify tubal factor infertility, as well as many organic pathologies of the reproductive system.
Hysterosalpingography is a method of hardware examination in gynecology. Using this technique, doctors determine the condition of the fallopian tubes, their morphological and anatomical features. The main purpose of the study is to determine the patency of the fallopian tubes.
Hysterosalpingography – what is it?
Having seen the entry in the doctor’s referral: HSG of the fallopian tubes, most patients do not have the slightest idea what this procedure is. This technique involves the examination of the uterine tubes and its appendages. The main parameter that doctors examine during this procedure is the patency of the uterine tubes. This factor has great value for successful and bearing a child. The method is often used to diagnose infertility in women with a long absence of pregnancy with active planning.
What does hysterosalpingography show?
Tubal hysterosalpingography allows doctors to evaluate the condition of one of the most important parts of the reproductive system from the inside. The meeting of male and female reproductive cells occurs directly in the fallopian tubes, so complete or partial obstruction of patency becomes an obstacle to normal conception.
In addition to pathologies of the fallopian tubes, gynecologists use hysterosalpingography to identify a number of other gynecological diseases:
- pathologies of the uterus - polyps, deformities, endometriosis, ;
- fallopian tube adhesions;
- cysts of the reproductive system;
- tumor-like processes in the uterus and its appendages (including malignant ones).

Hysteroscopy and hysterosalpingography - what is the difference?
The hysterosalpingography technique is based on the examination of the fallopian tubes and uterine cavity using an X-ray machine. The doctor injects a special contrast agent into the patient’s reproductive system, which helps to better structure the tissue. During the procedure, specialists take several photographs, which are then used to describe and diagnose possible pathologies of the reproductive system.
Hysteroscopy is a routine examination of the uterine cavity using a special optical device. This method cannot be used to obtain information about the condition of the fallopian tubes; they cannot be visualized using a hysteroscope. The main purpose of the method is to assess the condition of the uterine cavity and endometrium.
The method is used to identify the following uterine pathologies:
- polyps of the uterine cavity;
- cystic formations;
- inflammation of the endometrium.
Hysterosalpingography - indications
Testing of the fallopian tubes (HSG) can only be carried out on the direction of a doctor. The specialist decides on the need for research by analyzing the clinical picture and the patient’s complaints. Often the procedure is included in the list of examinations when diagnosing the cause of prolonged absence of pregnancy.
In addition, hysterosalpingography is prescribed by a gynecologist if there are suspicions of a number of pathologies and possible abnormalities in the development of the reproductive organ:
- violation of the anatomy of the uterus and appendages (, tortuous fallopian tubes);
- fibroids of the reproductive system;
- fallopian tube adhesions;
- cystic formations;
- polyps.
Hysterosalpingography – contraindications
Due to a number of contraindications, doctors are not always able to perform HSG: the patency of the fallopian tubes in this case remains in question. Before prescribing an examination procedure, the doctor carefully examines the patient’s condition, her medical history, and takes into account the presence of other pathologies and inflammatory processes in the woman’s body.
Hysterosalpingography is not performed in the following cases:
- pregnancy period (especially short periods);
- allergic reactions to a contrast agent (preliminary allergy tests for iodine-containing substances are carried out);
- history of uterine bleeding;
- inflammatory processes in the body, in the reproductive system and pelvis;
- period of exacerbation of chronic diseases;
- hyperthyroidism;
- thrombophlebitis;
- tumors and cysts in the uterus and appendages;
- viral and bacterial infections in the body.

HSG of fallopian tubes - preparation for the procedure
Preparation for fallopian tube HSG should begin 7 days before the study. From this moment on, the woman must stop all douching, use of intimate hygiene products, vaginal creams, and suppositories. Three days before the scheduled procedure, it is necessary to exclude sexual intercourse. The procedure is performed on an empty stomach. Before undergoing HSG, a woman must undergo a series of examinations. The list of them may differ in different clinics.
In most cases, before hysterosalpingography is performed, preparation for the procedure involves passing the following tests:
- blood test;
- testing for syphilis, HIV, hepatitis;
- urine test;
- on the vaginal flora;
- cytological scraping of the cervix.
On what day is a fallopian tube HSG performed?
For women undergoing hysterosalpingography, the gynecologist will tell you which day of the cycle to have it done. He directly sets the time and day for the procedure. The timing of its implementation is determined by the type of pathology. However, in most cases, doctors believe that best time for the study is the period from the beginning of the cycle (after menstruation) until ovulation. So, for women with a menstrual cycle of 28 days, the optimal time for examination is 6–12 days after menstruation. If indicated, doctors conduct an urgent examination on any day except during menstruation.
Hysterosalpingography – what to take with you?
Hysterosalpingography, HSG, does not require special devices or items for the woman. All you need to take with you is a diaper or a large towel. Some doctors recommend bringing sanitary pads. They are necessary because after the procedure they are often copious discharge from the vagina. Everything else will be given to the patient at the clinic where the examination procedure will be carried out.
Hysterosalpingography – does it hurt?
The main question for women undergoing examination for the first time concerns whether hysterosalpingography is painful. In most cases, the manipulation is performed without the use of anesthesia. In this regard, patients may experience some unpleasant sensations:
- pain in the lower abdomen;
- light stretching in the groin, as during menstruation;
- discomfort in the pelvic area.
To exclude this, some medical institutions perform the procedure under local anesthesia. In some cases, the patient may be asked to take an antispasmodic drug. It helps reduce muscle tension and contractility and reduce pain. Women who are very worried about the procedure are given a sedative the day before.

How is hysterosalpingography performed?
When receiving a referral for examination, a woman wants to familiarize herself with the algorithm of the procedure. How is HSG of the fallopian tubes done, how long does the manipulation last, is the pain severe - the answers to these questions will have to be given by the doctor who refers the woman for examination.
When talking with the patient, doctors pay special attention to important preparation rules:
- On the eve of the study, it is recommended to do an enema to completely cleanse the intestines.
- On the day of the study, you are prohibited from eating.
- 1.5 hours before the examination, you can drink a glass of still water.
- If hysterosalpingography is performed using ultrasound, the woman, on the contrary, will have to drink a lot of fluid to fill the bladder.
X-ray hysterosalpingography
GHA x-ray of the fallopian tubes is one of the first methods for examining them. Directly with its help, gynecologists for a long time established the condition of the fallopian tubes and uterine cavity, and diagnosed tubal infertility. The method consists of introducing a special solution into the uterine cavity, which fills the main organ of the reproductive system and gradually penetrates the tubes. Doctors receive the most detailed images and evaluate the organ from the inside.
The algorithm boils down to the following:
- The patient is located in a gynecological chair.
- The doctor installs speculum and cleans the vaginal cavity using sterile swabs.
- A special cannula is inserted into the cervical canal, through which a contrast agent is supplied.
- The speculum is removed and the uterine cavity is filled with contrast through a special catheter for hysterosalpingography.
- Afterwards, the woman is asked to lie down on a special table, above which there is an X-ray machine.
- The doctor takes pictures at a certain interval, which are then used to evaluate the process of movement of the substance through the fallopian tubes.
Ultrasound hysterosalpingography
Ultrasound, or as it is also called, ECHO HSG of the fallopian tubes, involves examining the reproductive system using ultrasound. The principle of the study itself is similar to that discussed above, however, instead of a contrasting solution, saline solution is used. On the monitor screen of the ultrasound machine, the doctor is able to visualize the fallopian tubes and the injected solution. If it reaches them and penetrates the abdominal cavity, the fallopian tubes are passable and there are no pathologies. Otherwise, the doctor in the conclusion indicates the degree of damage and the nature of the changes.
Hysterosalpingography is normal
After the HSG procedure of the fallopian tubes has been performed, the doctor carefully studies the information received. The conclusion indicates not only the degree of patency, but also the main parameters of the fallopian tubes. The documents issued to the woman are accompanied by several photographs, which clearly show possible violations. If necessary, the entire course of the procedure is recorded on disk.
The conclusion of a normal hysterosalpingography indicates the following information:
- the uterine cavity has the shape of an isosceles triangle with a base of 4 cm;
- fallopian tubes are contrasted on both sides;
- the ampullary section of the fallopian tubes is within normal limits;
- the contrast agent penetrates into the abdominal cavity.
HSG of fallopian tubes - consequences after the procedure
If HSG of the fallopian tubes is performed correctly and competently, the consequences of the procedure for the woman’s body are practically excluded. Minor discomfort, reminiscent of pain on the eve of menstruation, along with light pink discharge, is normal. After 2-3 days from the moment of examination, they completely disappear.
Doctors are of great concern possible complications GHA. The main one among them is allergic reactions to the contrast agent. In addition, the use of a large volume of contrast can lead to the fact that it begins to penetrate into the capillaries, lymphatic vessels, as well as into the venous network of the reproductive organ. Excessive fluid administration can cause fallopian tube rupture, which requires emergency medical attention.
Pregnancy after tubal HSG
Doctors prohibit planning a pregnancy after hysterosalpingography in the cycle following the procedure. This is due to the possible negative impact of contrast and x-rays on a woman’s reproductive system. In the case of HSG using ultrasound, these restrictions do not exist.
In general, women after hysterosalpingography, in the absence of tubal obstruction, can freely plan conception. When, during the study, adhesions and other formations that violate the condition are discovered, doctors prescribe complex treatment.