Chapter 1. Intestinal infections
Chapter
Introduction.
Infectious morbidity occupies one of the leading places in the field of medical, social and economic problems of our time. This is evidenced by the national program for combating infectious diseases developed and operating in our country. Currently, the incidence of infectious diseases remains at a high level and there is no noticeable tendency to decrease it.
Infectious diseases is a discipline that studies the clinical manifestations of an infectious process in a patient. This discipline is closely related to epidemiology, a discipline that studies trends in the development of the epidemic process at the population level.
In medical practice, there are frequent cases when patients with infectious diseases are initially hospitalized in non-infectious hospitals (therapeutic, surgical, etc.). In this regard, medical personnel, including nurses, must have a good understanding of the patterns of occurrence, development and course of infectious diseases, the principles of their diagnosis and treatment. Therefore, the role of paramedical workers in the prevention of infectious diseases is not only constantly becoming more complicated, but also expanding. Currently, much attention is paid to the role of a nurse, not only in organizing nursing care for infectious patients, but also in compliance with the anti-epidemic regime.
The basis for the prevention of infectious diseases is the immunization of the population, which reduces the incidence, mortality and mortality from a number of infections.
So, for example, in 2013 alone, 18008 cases of AEI were registered in the Khanty-Mansi Autonomous District, the incidence rate of intestinal infections was 1135.4 per 100 thousand population, which is almost 1.05 times higher (1086.4) compared to the same period in 2012. The greatest increase in the incidence of intestinal infections was noted in January-April 2013.
As an example, we can consider such diseases as salmonellosis and dysentery. Thus, the consistently high incidence of salmonellosis, which remains one of the most pressing problems of the sanitary and epidemiological well-being of the district, the incidence of salmonellosis is 2.35 times higher than the average level in the Russian Federation (33.65 per 100 thousand population).
In 2013, 1256 cases of salmonellosis were registered in the Khanty-Mansiysk Autonomous Okrug-Yugra, the intensive rate was 79.19 per 100 thousand of the population, compared to 2012, there was a decrease of 14.3%. In 2013. there was a decrease in morbidity in all age categories: the adult population by 11.5%, the child population under 17 by 18.7%. (Appendix No. 1)
The high incidence of salmonellosis, data from laboratory studies of poultry raw materials and products indicate that the Autonomous Okrug continues to supply products that do not meet safety requirements.
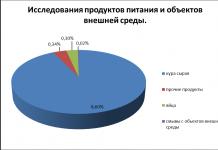
In order to monitor the circulation of Salmonella in the territory of the Autonomous Okrug, research is being carried out on food products and environmental objects. (Appendix # 2) 22897 samples for salmonellosis were examined, positive findings were found in 80 cases (0.35%), including:
Raw chicken - 489 samples - 42 positive findings (8.6%),
Other products - 9583 samples - 33 positive findings (0.34%),
Eggs - 668 samples - 2 positive findings (0.3%),
Washes from environmental objects 12157 washes - 3 positive findings (0.02%).
In 2013, 149 cases of dysentery were detected, which is 1.28 times more than in the same period in 2012. (115 cases). In the structure of dysentery infection in 2013. the specific gravity of the tank of confirmed dysentery is 92.0%, among which dysentery was 59.8% (an increase of 42.0% compared to 2012), Flexner's dysentery was 35.0% (a decrease of 22.1% compared since 2012).
In the etiological structure of AEI of the established etiology, as in previous years, enteric viruses predominate, their share increased from 29.9% in 2002 to 70.9% in 2013. In 2013, rotaviruses, noroviruses, adenoviruses and astroviruses were diagnosed. Rotavirus infection dominated in the etiological structure of AEI of the established etiology. During 2013 3605 cases were registered, incl. 3298 cases among children. The incidence rate of rotavirus infection in 2013 was 227.3 per 100 thousand population, which is 17.7% lower than the incidence in 2012. The 2nd place among all viral intestinal infections is occupied by OCI caused by the Norwalk virus. Also, in 2013, the incidence of acute intestinal infections of unknown etiology was 580.7 per 100 thousand of the population and decreased by 4.2% compared to 2012 (605.3), respectively.
Future nurses should be professionally oriented in infectious pathology and the basics of epidemiology, successfully apply their knowledge and skills in practice.
This paper sets out ideas about the responsibilities of nursing staff of an infectious medical institution, about the prevention of infectious intestinal diseases. Also arising in connection with this, the duties and peculiarities of the work of a nurse of a medical and preventive institution of this profile.
Based on the above statistical data, I set the goal of the work - to find out the role of a nurse in diagnostic and treatment measures for intestinal infections (for example, salmonellosis).
To solve this goal, I solved the following tasks:
Determine the form of presenting information to patients in an understandable and accessible form with a full explanation of the essence of the planned and ongoing interventions.
Find out what medical and diagnostic interventions for intestinal infections are carried out in the Khanty-Mansi Autonomous Okrug (for example, salmonellosis)
Determine possible complications when taking medications used in the treatment of intestinal infections (for example, salmonellosis).
Determine the features of preparation for various types of research carried out in the course of the medical and diagnostic process.
The practical significance of this topic is to increase the awareness of the population about the prevention and complications of intestinal infections using the example of salmonellosis.
Chapter 1.Overview of intestinal infections and salmonellosis.
Nurse participation in treatment activities
Hospitalization of patients is carried out only in case of severe or complicated course, as well as for epidemiological indications. Bed rest is prescribed for severe manifestations of toxicosis and dehydration.
If the patient's clinical condition allows, treatment should be started with gastric lavage, siphon enemas, and the appointment of enterosorbents (activated carbon, etc.)
Regime and nutrition for salmonellosis
Treatment of salmonellosis in adults begins with adherence to bed rest. In the case of moderate and severe forms - ward bed rest. For patients with salmonellosis, a special diet No. 4 has been developed. (Appendix No. 6) All products that irritate the stomach, including dairy products and refractory fats, have been excluded.
Application form
What intestinal infections do you know? ____________________________________________________
Do you have any diseases of the gastrointestinal tract? ____________________________________________________
If yes, how do you undergo medical treatment courses under the supervision of your doctor, or do you self-medicate? __________________________________________________________
Do you have diarrhea or bloating? __________________
If yes, what are you doing to correct these symptoms? ________________________________________________
Do you have any chronic diseases? ____________
Are you on a diet? Which one? _____________________________
How many times a day do you eat? ______________________________
What kind of food do you prefer (home, fast food, etc.)? ____________________________________________________
Did you know that it is better to wash food in boiled water before use? ___________________________________________
How many times a day do you brush your teeth? __________________________
Remember and write down the rules for safe food ________________________________________________________________________________________________________________________________________________________________________________________________________________________________
Date of completion _____________
For additional information of the population with a preventive purpose, it is necessary to conduct conversations with the population, as well as to publish and distribute leaflets on the prevention of salmonellosis and recommended methods of food processing. As an example of a reminder for the prevention of salmonellosis, I suggest using the following option.
REMINDER
Why is salmonellosis dangerous?
It is one of many acute intestinal diseases characterized by a sharp rise in temperature up to 38-39 ° C, abdominal pain, vomiting and diarrhea. Anyone who has experienced similar symptoms at least once can say that this condition is not pleasant. It should also be noted that if you do not seek medical help in time, the result of this disease can be quite deplorable, because vomiting and loose stools lead to dehydration of the body, which can cause heart problems, and the released toxins damage internal organs. And this is especially dangerous for the elderly and young children. But mostly they are sick with salmonellosis.
Who is she - this mysterious Salmonella and where does she live?
Salmonellosis is a disease that is caused by different types of bacteria (Salmonella of different groups) that live in different conditions. Therefore, one should not be sensitive to egg products and at the same time calmly eat non-salted lard with full confidence that you will clearly not get infected with salmonellosis. This is not true. And you need to be careful with any type of food.
Previously, it was believed that the main transmission factor in half of those with salmonellosis was chicken eggs cooked at home - these are scrambled eggs, and omelets, and boiled soft-boiled eggs, as well as eating raw chicken eggs. But this is only a small part, because not fried grilled chickens, and home-made salads, and raw dough mixed with eggs can also serve as a source of infection. Here the violations are obvious: you cannot eat raw foods, be it eggs or dough. Everyone knows about it. If you see that the same grilled chicken is not overcooked, it is better to discard it, throw it away or, in extreme cases, bring it to readiness already at home. Believe me, the treatment will cost much more.
In isolated cases, transmission factors are raw goat milk and lard. And the fault is the same violation of the cooking technology. After all, milk must be boiled, and lard must be salted well.
However, despite the fact that chickens and eggs are the main source of salmonellosis, it is impossible to identify any one manufacturer (and, accordingly, take action). All the products that caused the disease are produced by different manufacturers and in different places. Therefore, the phrase “Your health is only in your hands” takes on special seriousness.
The solution to this issue is quite simple. After all, for this you just need to remember and observe the usual rules of hygiene, which are familiar to every person from childhood, and also always remember about common sense. In fact, all the rules listed below apply not only to salmonellosis, but also to other intestinal infections and poisoning in general. Let's remember them:
Be sure to wash your hands with soap and water after using the toilet and before eating.
Ask yourself a question: is it possible to eat semi-raw foods and of course you will answer yourself: "NO, NOT". And if you see that meat or chicken is not cooked or cooked, do not be lazy, continue cooking them. These simple steps guarantee not only your safety, but also the taste of the dish.
Do you have a refrigerator? Of course yes". Therefore, always all ready-made products (especially salads, products with minced meat or cream) should be stored only in the refrigerator. Otherwise, they may simply deteriorate, and you risk getting food poisoning.
Purchase several cutting boards and define a rule for yourself: "Raw and prepared foods must be cut on different boards and with different knives." Indeed, even if some bacteria live in raw chicken, it will not survive during the cooking process: when boiling or roasting. But if you make a salad on the same board where you cut up the chicken, all the salmonella from the chicken will end up on your plate.
And one more question: how often do you pay attention to expiration dates on food packaging? Yes, yes, and again the rule: "Carefully look at the expiration dates and storage conditions of products in stores." If the same meat is stored in a display case without refrigeration, in the heat, and even under the sun - think twice and thrice whether your health is worth risking.
Pay attention to how the seller weighs the products. Do not buy groceries in a store where the seller weighs chickens and sausages on the same scales, that is, raw and finished products. Nothing will happen to chickens, but such a sausage is very easy to poison.
If it seemed to you that the product is spoiled, that the salad bought or made a day ago gives off sourness, that the chicken or meat remained raw inside - do not eat. Throw it away. No matter how sorry it is. Believe me, the treatment will cost much more than the same chicken. Not to mention what you have to endure in case of illness. After all, you deserve more than a sour salad.
Do you know how important it is to wash chicken eggs? Yes, yes - wash the chicken eggs. It is very important. Moreover, you need to wash them not immediately before cooking, but as soon as you brought them from the store. And only then put it in the refrigerator for storage. There are often cases when Salmonella is introduced onto food again: it remains on a hand towel, a spatula for cooking or on a knife used to break eggs. And the result is still sad.
And one more piece of advice that requires your special attention: no matter how much you would like to pamper your baby with scrambled eggs or an omelet - stop and think. Our advice to you: "Do not feed small children with eggs", because it is small children from birth to 2 years of age that make up exactly one third of all patients with salmonellosis. The disease is dangerous for them and is usually quite difficult. Do not expose your children to this kind of danger. Do not feed them raw eggs. Do not give them food that you are not sure of.
Take care of the health of your loved ones and be healthy yourself!
For preventive work with the population, it is recommended to publish and distribute leaflets with general information on the prevention of Oka (Appendix No. 9)
I have developed a project that includes additional ways of informing the population on issues related to the problem of salmonellosis. At the present stage of development of society, I consider it possible to develop and create a page on social networks, send SMS to phones, send newsletters to e-mail addresses, a video before a movie in a cinema, distribute electronic brochures on the internal network (as agreed with the manager).
To achieve the goal of identifying possible complications when taking medications used to treat salmonellosis, I studied the treatment process, and the features of the rehabilitation period after the illness. In this connection, it should be noted that the main side effects of the drug "Enterosgel" used to treat salmonellosis are symptoms such as nausea, constipation. In severe renal or hepatic impairment, a feeling of disgust for the drug may appear. In order to reduce and eliminate which, after the transferred disease, the rehabilitation (recovery) stage should be properly organized, which plays the most important role in the recovery process of the body.
In the course of the survey, it was also found that patients are least informed about the correctness of preparation for examination on the prevention of intestinal infections. In this connection, I propose to publish thematic memos on the correct preparation for the examination, including the rules for collecting material for the feces sowing tank.
Conclusion.
In different countries, various infections are widespread, and their incidence is greatly influenced by the social conditions of people, the consciousness of people, and the observance of the rules of personal hygiene. The higher the social and cultural level of the population, the organization of preventive and curative care, health education, the lower the prevalence of infectious diseases and mortality from them. Infectious diseases are one of the leading health problems and are the third most prevalent worldwide after diseases of the cardiovascular system and tumors.
The reasons for the spread of infectious diseases are population growth, demographic stratification and the intensity of migration processes.
At the present stage of the development of infection and the existing epidemiological situation, the nurse should know the clinical picture of intestinal infections. Be able to conduct conversations in an accessible form for the patient, draw up memos and make newspaper walls.
When solving the set tasks, using the example of such an intestinal infection as salmonellosis, it was found that intestinal infections are found among all age groups, both among the local and among the visiting population. All the tasks were completed. I developed and presented a project for the prevention of intestinal infections, as well as joint work with the center of occupational pathology: issuing brochures on the prevention of intestinal infections, developing newspaper walls.
Bibliographic list.
1. Antonova T.A. and other Infectious diseases. 2000 g
2. Vasiliev V. S. Practice of an infectious disease specialist. 1993 year
3. Malov V.A. Nursing for infectious diseases. 2005 year
4. Mukhina S. A. and others. General patient care. 1989 year
5. Obukhovets T.P., Sklyarova T.A., Chernova O.V. The basics of nursing care. 2000 g
6. Modern medicine. Directory. Diseases. Syndromes. Symptoms Moscow ONYX 21st Century, Peace and Education. 2004 r.
7. Obukhovets T.P., Sklyarova T.A., Chernova O.V. The basics of nursing care. 2000 g
8. Podlevsky A.F. Infectious Diseases Office Nurse. 1988 year
9. Rubashkina L.A. other. Infectious diseases with a course of HIV infection and epidemiology. 2002 year
10. Titarenko R.V. Nursing in infectious diseases and the course of HIV infection and epidemiology. - Rostov-on-Don: Fentx, 2009.
11. Shuvalova EA Infectious diseases. Phoenix, Rostov-on-Don. 2001 year
13. Modern medicine. Directory. Diseases. Syndromes. Symptoms Moscow ONYX 21st Century, Peace and Education. 2004 year
14.http: //www.medlinks.ru/sections.php?op=viewarticle&artid=1066
Appendix No. 1
Appendix # 2

Appendix No. 3

Appendix No. 4
General urine analysis
Target. Determination of the number of formed elements in 1 ml of the average portion of urine collected during urination.
Equipment. Rubber gloves, a towel, a clean dry jar with a label for urine, a referral form to the laboratory.
Mandatory conditions. For the study, an average portion of morning urine is taken (during urination), which prevents the ingress of uniform elements from the lower parts of the urinary system, as well as from the genitals, into it.
Advantages. Eliminates the need for bladder catheterization.
1. Establish psychological contact with the patient. Explain to him the purpose and course of the procedure, obtain consent.
2. Prepare the necessary equipment, write a referral to the bacteriological laboratory.
3. We warn the patient that before the fence it is necessary to wash the genitals
4. Then we explain to the patient that he should collect the middle portion of urine in a clean, dry jar.
5. Take 10 ml of urine for research.
6. Arrange the transportation of the received material to the laboratory within an hour.
Appendix No. 5
Appendix # 6
What foods can be consumed:
1. Bread, flour products: dry rusks. from thinly sliced premium wheat bread.
2. Soups: on a weak meat, fish broth (fat-free), with the addition of rice or semolina mucous broths, egg flakes, steamed meatballs and dumplings, boiled, grated meat.
3. Meat and poultry: non-stringy and lean varieties of veal and beef, chicken, rabbits.
4. Fish: fresh fish of low-fat species in a piece or in the form of minced products - cutlets, meatballs, dumplings, boiled in water or steamed.
5. Dairy products: steamed soufflé, freshly made grated cottage cheese.
6. Fats: exceptionally fresh butter, at the rate of 5 g per serving (only for ready meals).
7. Eggs: steam omelette, soft-boiled, for cooking. A total of one or two for the whole day.
8. Vegetables: exclusively in the form of decoctions for making soup.
9. Cereals: only pureed porridge, cooked in fat-free broth.
11. Sweets, fruits, sweet dishes: jelly and jelly from quince, bird cherry, pear, dogwood, blueberry. Mashed raw apples.
12. Drinks: cocoa, black coffee, tea (especially green), decoctions of quince, black currant, wild rose, bird cherry, dried blueberry.
13. Spices and sauces: only fat-free broth and butter added to dishes.
Diet number 4 - what foods should not be consumed
1. Flour products: other flour and bakery products other than those indicated above.
2. Soups: fatty, strong broths, dairy soups, as well as with vegetables, cereals, pasta.
3. Meat and poultry: fatty meat, whole piece, sausages, sausages and other meat products.
4. Fish: canned fish, caviar, salted and fatty fish.
5. Dairy products: whole milk and other dairy products.
6. Fats: other fats and oils.
7. Eggs: raw, hard-boiled and fried.
8. Vegetables: all vegetables fresh, boiled and otherwise.
9. Groats: barley groats, pearl barley, millet, legumes, pasta.
10. Snacks: completely excluded.
11. Sweets, fruits, sweet dishes: all dried fruits, in their natural form.
12. Drinks: with milk - cocoa and coffee, cold drinks, all carbonated drinks, kvass.
Appendix No. 7
Conversation on the topic: Prevention of intestinal infections.
Intestinal infections include dysentery, typhoid fever, paratyphoid fever A and B, cholera, gastroenteritis, foodborne infections, viral hepatitis A, viral diarrhea. For all these diseases, the penetration of pathogens through the mouth and their multiplication in the human intestine is characteristic, from where they again enter the external environment with feces: soil, water, on various objects and food. The causative agents of acute intestinal infections are highly resistant in the external environment. The causative agents of dysentery retain their viability for several months on contaminated dishes, for several days on food (milk, meat products, bread, vegetables, fruits), up to 5-6 days, in water. The causative agent of cholera (Vibrio cholerae) can persist in the soil for 2 months, in running water - up to several months, on vegetables, fruits - up to several days, in raw milk - more than a week. The causative agents of typhoid fever, colienteritis, viral hepatitis are even more resistant in the external environment. In milk and dairy products, pathogens not only persist, but also actively multiply, without changing the appearance and taste of the product. But when exposed to high temperatures, microbes die. When boiled, the causative agents of dysentery die instantly, causative agents of cholera - within a minute, causative agents of hepatitis - within 30-40 minutes.
The source of acute intestinal infections is a person who is sick or a carrier of bacteria.
The carrier bacterium is a practically healthy person, in whose body there are pathogens of intestinal infections. The susceptibility of people to acute intestinal diseases is quite high. Children are especially susceptible to them.
The greatest rise in the incidence of intestinal infections is observed in the summer-autumn period, which is associated with vacations, an abundance of vegetables and fruits, street trade in perishable food, violation of the water regime, etc. Human infection occurs if pathogens enter the intestines through the mouth. Food contamination can occur when contaminated with hands, as well as improper transportation and storage. Foods consumed cold, without heat treatment, are dangerous: salads, aspic, milk and dairy products, as well as semi-finished meat products. The causative agents of acute intestinal infections can also be found on the surface of vegetables, berries, and fruits.
One of the ways of spreading acute intestinal infections is water. Thawed, rainwater wash away pathogens from the surface of the earth into open water bodies, rivers, lakes, ponds. You can use melt water for drinking, washing dishes, hands, vegetables and fruits only in boiled form. Contamination with this water is not excluded when bathing.
The cause of acute intestinal infections can also be water from the well, if the well is improperly built or used incorrectly (there is no clay castle, the well is located near the latrines, residents take water with individual buckets, wash clothes and dishes in the immediate vicinity of the well)
Appendix No. 8
"Parents, be careful - an intestinal infection is better to prevent than to cure."
· Strictly observe the rules of personal hygiene, often and thoroughly wash your hands with soap and water, especially before eating and after using the toilet;
· Use boiled, bottled water.
• Wash vegetables, fruits, berries thoroughly before use under running tap water, and for small children - boiled;
· Use only clean packaging (polyethylene, food containers, etc.);
· Do not purchase food products from random persons or in places of unauthorized trade;
· Observe the rules of hygiene when preparing hot and cold dishes, shelf life and storage conditions of food, especially perishable, raw food and ready-made food should be stored separately;
· Thoroughly fry or boil food, especially meat, poultry, eggs and seafood;
· Perishable food and prepared food should be stored only in the refrigerator at a temperature of 2-6? С;
· Do not mix freshly prepared food with the leftovers from the previous day, but if the prepared food remains the next day, then before use it must be subjected to heat treatment (boil or fry).
· Do not accumulate garbage and food waste, do not allow flies and cockroaches to appear, constantly keep the home clean and follow the rules of personal hygiene, do not give young children unboiled draft milk, raw eggs, use only fresh food for cooking.
Appendix No. 9
Patient reminder
for the prevention of acute intestinal infection
Acute intestinal infections (ACI)- a group of infectious diseases caused by various microorganisms (bacteria, viruses) united by a similar nature of clinical manifestations in the form of gastrointestinal dysfunction and symptoms of extraintestinal disorders.
These include:
Dysentery;
· typhoid fever;
• paratyphoid fever A and B, cholera;
· Salmonellosis;
Enterovirus infections, etc.
The source of infection is a sick person and a carrier of AEI pathogens. Both adults and children are ill (especially children from 1 to 7 years old).
The main route of transmission is fecal-oral. Transmission factors can be: food, water, household items, toys.
Symptoms are acute, with fever, vomiting, upset stools, bloating and abdominal pain. They can occur both on the first day after infection and on the seventh day (this is how long the incubation period of the disease lasts).
AEI prevention measures.
1. Observance of personal hygiene, thorough washing of hands with soap before meals and after visiting public transport, toilets (after all, after washing hands, the number of microorganisms is significantly reduced).
2. Do not drink water from open sources or sold in spill on the street. Boil your water!
3. Before eating fresh vegetables, wash them thoroughly and pour boiling water over them.
4. For nutrition, choose foods that have been cooked, thoroughly fry (boil) foods, especially meat, poultry, eggs and seafood. Do not store food for long, even in the refrigerator.
5. Do not leave cooked food at room temperature for more than 2 hours. Do not eat foods that have expired and that have been stored without cold.
6. Avoid contact between raw and prepared foods.
7. Swim only in the places established for this purpose. When swimming in ponds and pools, do not allow water to enter your mouth.
Following these simple tips will help you avoid acute intestinal infection and preserve your health and the health of your loved ones!
But, if you suddenly develop symptoms of acute intestinal infection (OCI), you should immediately seek medical help!
Always be healthy!
Appendix No. 10
The use of bacteriophages.
Phages are also used for treatment and prevention a number of bacterial infections. Produce typhoid, salmonella, dysentery, pseudomonas aeruginosa, staphylococcal, streptococcal phages and combined preparations (coliprotein, pyobacteriophages, etc.). Bacteriophages are prescribed according to indications orally, parenterally or locally in the form of liquid, tablet forms, suppositories or aerosols.
BACTERIOPHAGES - live agents, bacteria viruses, widespread in nature. In medicine, the ability of bacteriophages to destroy the cells of pathogens is used. The lytic action of bacteriophages is strictly specific.
In the production of phage preparations, the specificity of bacteriophages is taken into account and polyvalent phage preparations are prepared, namely, mixtures of bacteriophages that are active against various types of pathogens.
Advantages of bacteriophage preparations:
- highly effective biological preparations of antibacterial action for the prevention and treatment of acute intestinal infections and pyoinflammatory diseases, treatment of dysbacteriosis;
- when applied, they do not violate the normal human biocenosis;
- are indispensable for the resistance of pathogens to antibiotics;
- can be used in combination therapy with other drugs;
- are necessary in the treatment of dysbiosis in combination with drugs that normalize the intestinal microflora;
- recommended for adults and children;
- are made using natural raw materials.
Appendix No. 11
Stool analysis for i / g
PURPOSE
Diagnostics and differential diagnosis of diarrheal infections, helminthiasis and protozoal invasions, assessment of the severity of complications.
INDICATIONS
All patients of the infectious diseases hospital undergo a bacteriological examination of feces. To diagnose a violation of colon microbiocenosis, the composition of the fecal microflora is examined.
Coprological examination in patients with infectious diseases is performed:
To identify the inflammatory process;
To identify intestinal bleeding;
For the diagnosis of disorders of digestion and absorption of food;
For the diagnosis of helminthiasis and protozoal infections.
CONTRAINDICATIONS
There are no contraindications for the study,
PREPARATION FOR RESEARCH
In the absence of urgent indications for 3-5 days, the patient receives a standardized diet (Pevzner, Schmidt), if microbleeding is suspected for 2-3 days - a diet that does not contain meat, fish, poultry, green vegetables, tomatoes, as well as iron supplements ...
Introduction ………………………………………………………………………… ... 3
Chapter 1. Intestinal infections
1.1. Classification of intestinal infections ……………………………… .. …… ..7
1.2. Causes and risk factors of intestinal infections ...................... ... ...................... 10
1.3. Functional duties of the medical department of the infectious diseases ward ..................... 12
1.4. Salmonellosis ……………………………. …………………………………. 18
1.5 Participation of m / s in diagnostic measures for salmonellosis ........ 22
1.6. Participation of m / s in medical measures .................................. 24
Chapter 2. The participation of a nurse in the prevention of intestinal infections.
2.1. Questionnaire on the awareness of patients about salmonellosis .... 26
2.2. How to prevent the occurrence of acute intestinal diseases ... ... ... 30
2.3. How to avoid salmonellosis …………………………………………… .32
Conclusion ……………………………………………………………………… .37
Bibliographic list …… .. …………………………………………… 38
Appendix No. 1 ……………………………………………………………… .39
Appendix No. 2 ……………………………………………………………… ..39
Appendix No. 3 ……………………………………………………………… ..40
Appendix No. 4 ……………………………………………………………… ..41
Appendix No. 5 ……………………………………………………………… ..42
Appendix No. 6 ………………………………… .. ……………………………… 44
Introduction.
Infectious diseases have always been in the past and remain today one of the leading health problems. According to the WHO, about 33% of people die from infectious diseases.
Output data of the collection:
EPIDEMIOLOGICAL ASSESSMENT OF POSSIBLE RISK FACTORS OF INTESTINAL INFECTION
Isakova Zhainagul Turganbaevna
Lecturer at the Department of General and Clinical Epidemiology, KSMA named after I.K. Akhunbaeva, Republic of Kyrgyzstan, Bishkek
Toygombaeva Vera Sadvakasovna
Dr. med. Sci., Professor of the Department of General and Clinical Epidemiology, KSMA named after I.K. Akhunbaeva Republic of Kyrgyzstan, Bishkek
Alymkulova Venera Alymkulovna
Lecturer at the Department of General and Clinical Epidemiology, Republic of Kyrgyzstan, Bishkek
ANNOTATION
The article presents the data of a sociological survey of students about the presence of bad habits, the nature of water consumption, compliance with the rules of personal hygiene and knowledge about the factors of transmission of intestinal infections.
Keywords: morbidity, intestinal infections, bad habits, risk factors.
Infectious diseases at the beginning of the 21st century are still one of the most important public health problems around the world. According to the WHO, more than 2 billion people suffer from infectious diseases every year, of which 17 million die. Every day in the world 50 thousand deaths are caused by infectious diseases, which are still the leading cause of death and the first cause of premature death.
Among infectious diseases the most common (after ARVI) are sharpintestinalinfections(OKI).
Disease frequency intestinalinfections, estimated in extended prospective studies over the past 50 years in the United States at 1.2 to 1.9 cases per person per year, the number of deaths associated with infectiousd iaarrhea, ranging from 500 per year atchildren up to over 10,000 in the adult population. The highest incidence is recorded in children young age: 2.46 cases of the disease per year per 1 child under the age of 3 years.
According to the WHO, more than 5 million die from AEI and their complications every year in the world. children. Despite the advances in medical science and practical health care, acute intestinal infections (AEI) remain one of the urgent problems of our time. According to the World Health Organization, up to 1-1.2 billion diarrheal diseases are annually registered in the world, from which about 4 million people die, and 60-70% of the cases are children under the age of 14 years. They pose the greatest threat to young children, due to the high level of morbidity and mortality among them. According to Russian authors, intestinal infections rank 3-4 among all infectious diseases in children. In addition to damage to public health, they cause serious economic damage. In the United States, economic losses from OKZ amounted to about $ 1.5 billion, in Russia - 253.45 billion rubles. ...
The problem of acute intestinal infections has completely retained its relevance for the Kyrgyz Republic due to the prevailing unfavorable socio-economic consequences - the disintegration of the former Soviet Union, a noticeable decline in living standards, unemployment, migration of the rural population from village to city and deterioration of sanitary and living conditions. In the structure of infectious pathology without influenza and ARVI in the Kyrgyz Republic, the share of intestinal infections is 49%. The high incidence of intestinal infections determines the importance of conducting epidemiological studies for the development of preventive measures, reducing socio-economic damage, and protecting the health of the child population.
Purpose of the study: epidemiological assessment of behavioral risk factors for intestinal infections of students.
Materials and research methods. The material for the study was the survey data conducted among the students of the capital's universities at the age of 17-22 years (500 pcs.).
Methods: statistical, search, sociological.
Discussion results. To assess the knowledge about the influence of behavioral risk factors on the spread of intestinal infections, we conducted a survey of students of the capital's universities. The questionnaire contained 20 questions, from the answers to which they received information about knowledge of the prevention of intestinal infections, the type of water supply, issues of personal hygiene, places of residence and the presence of bad habits.
The respondents were 500 students, of which 54.1 ± 2.2% were females, 45.9 ± 2.2% were males. Age ranged from 17 to 22 years (Fig. 1 and 2).
Figure 1. Share by age

Figure 2. Specific gravity by sex
To the question "Do you know how intestinal infections are transmitted?" the majority of respondents (76 ± 2.0%) answered positively. But among the students, there were also those who did not know about it - 23.7 ± 2.0% (Fig. 3).

Figure 3. The proportion of answers to the question "Do you know how intestinal infections are transmitted?"
When asked what kind of water they use, the respondents indicated that they use water from a central water source, and only 5.6 ± 1.0% of students noted that they use water from an open source (Fig. 4).

Figure 4. Type of water supply
One of the factors of possible intestinal infections are vegetables and fruits, which can be contaminated with soil. Therefore, our questionnaire contained a question about the rules for washing vegetables and fruits before eating them. As the answers showed, most students rinse them under running water. However, there were those who did not wash them at all - 2%, and 6.4 ± 1.1% of students scalded them with boiling water before use (Fig. 5).

Figure 5. The proportion of answers to the question "How do you wash vegetables and fruits?"
Behavioral risk factors for intestinal infections include bad habits. It turned out that about 30% of respondents have the following bad habits: biting and gnawing nails - 58%, putting a pen or pencil in your mouth - 35.8% and 7% - putting your fingers in your mouth.
The transfer of chewing gum to each other can also be attributed to bad habits, such were 2% of students.
To comply with the rules of personal hygiene, appropriate conditions are required at the place of study and residence. To the question "Are there conditions for hand washing in the educational institution?" 13% of the respondents gave a negative answer, which indicates that they do not have the opportunity to wash their hands during the day.
To the question "When do you wash your hands?" it turned out that 43.4 ± 1.5% of students wash before eating, 17.4 ± 1.2% after eating, and 39.2 ± 1.5% of students after visiting the toilet.
To identify the knowledge of students about possible routes of infection, we included the question of the factors of transmission of intestinal infections. 38 ± 1.5% of respondents believe that dirty hands are a factor of transmission, 25.4 ± 1.4% - vegetables and fruits, 15.8 ± 1.1% of cases can be infected in public transport, in 14.3 ± 1 , 1% - can be money, 6.2 ± 0.7% of respondents - when working on a computer (Fig. 6).

Figure 6. Share of transmission factors (%)
At the same time, it should be noted that the stereotypes of water consumption have changed. From these questionnaires, it turned out that 39% of students drink boiled water, which raises doubts. Filtered, raw and bottled water is consumed by 21.6 ± 1.6%, 20.0 ± 1.6% and 16.9 ± 1.5%, respectively (Fig. 7).

Figure 7. Specific weight of the nature of water consumption (%)
Conclusions:
1. The problem of acute intestinal infections has fully retained its relevance for the Kyrgyz Republic due to the prevailing unfavorable socio-economic consequences. In the structure of infectious pathology in the Kyrgyz Republic, the proportion of intestinal infections without influenza and ARVI is 49%.
2. Among the respondents, women accounted for 54.1 ± 2.2%, men - 45.9 ± 2.2%.
3. 80% of students are well informed about the ways and factors of transmission of intestinal infections.
4. Bad habits are one of the reasons for the spread of intestinal infections, which affect 30% of the respondents.
5. According to our research, possible factors of transmission of intestinal infections are 38 ± 1.5% - dirty hands, 25.4 ± 1.4% - vegetables and fruits, 15.8 ± 1.1% - public transport, 14, 3 ± 1.1% - money, 6.2 ± 0.7% - computer.
Bibliography:
1. Aidaraliev A.A. Scientific bases of optimization of the system of training health management personnel in the Kyrgyz Republic at the present stage: Diss. for the degree of Doctor of Medical Sciences: 14.00.33. Bishkek. 2002 .-- 33 p.
2. Briko N.I., Pokrovsky V.I. Globalization and the epidemic process. / N.I. Briko, V.I. Pokrovsky // Epidemiology and infectious diseases. - 2010. - No. 4. - p. 4-10.
3. Kasymbekova K.T. Epidemiology of enteric viral infections in the Kyrgyz Republic: Dissertation for the degree of Doctor of Medical Sciences: 14.0030. M. 2004 .-- 35 p.
4. Onishchenko G.G. the fight against infectious diseases is a priority topic of the chairmanship of the Russian Federation in the G8 in 2006. // Health of the Russian Federation. - 2007. - No. 1. - S. 3-6.
5. Shakhanina I.L. Economic damage caused by infectious diseases in the Russian Federation as of December 2000 / I.L. Shakhanina, L.A. Osipova, O. I. Raduto // Epidemiology and infectious diseases. - 2001 - No. 6. - P. 58.
Municipal budgetary educational institution
"Center for extracurricular activities" in Bryansk
International Research Conference for Students and Teachers "First Steps to Science"
Research
"Dynamics and spread of diseases of the gastrointestinal tract
among children and adolescents of the city of Bryansk "
Subject area: Medicine (additional education)
Syomachkina Julia
MBOUDOD "CVR", Bryansk,
Association "Home nurse"
Supervisor:
additional education teacher
Introduction ………………………………………………………………………… ... 1
Chapter 1. Diseases of the gastrointestinal tract ………………………… ... 3
1.1. Characteristics of diseases …………………………………………… ... 3
1.2. Etiology of diseases …………………………………………………… 3
Chapter 2. Analysis of diseases of the gastrointestinal tract among children and adolescents of the city of Bryansk ……………………………………………………… 3
· One third of the interviewed people have gastrointestinal diseases.
· Not all families enjoy a varied diet.
· Some middle-aged schoolchildren do not know which foods are healthy.
· A quarter of the interviewed people often eat fast food and have bad habits.
· Only one third of the respondents consider their state of health to be good.
· Most of all, stress, unhealthy diet, environment worsens the state of health.
3.2. Prevention of diseases of the gastrointestinal tract
1) Observe the nutritional conditions and regime. Frequent meals, divided into small portions, will be helpful.
2) Eat a proper diet. It will be useful to reduce the consumption of fried, fatty, smoked, salted foods. It is necessary to increase the fiber content in the diet (vegetables and fruits, bran bread, cereals). Eat as much coarse fiber food as possible, fresh salads, try to use less vinegar and similar ingredients when cooking.
3) Avoid overeating. Eat in moderation, remember that a standard portion of food should not exceed 300-400 ml if presented in a liquid state. On the other hand, you cannot force yourself to starve, you need to eat in an orderly and healthy way.
4) Control your body weight. If you are overweight you should try to lose weight. Remember that this must be done correctly: weight loss should not be more than 0.5 kg for women and 1 kg for men per week.
5) Give up bad habits.
6) Learn to deal with stressful situations. Try not to get nervous, go for a walk, rest and get enough sleep.
7) Limit carbonated drinks and coffee.
8) Move more.
Conclusion
Diseases of the gastrointestinal tract do not spare anyone: neither children nor adults. We notice more and more clearly how these diseases are "getting younger". Already at an early age, diseases of the gastrointestinal tract are formed and, unfortunately, no positive dynamics is observed. Over time, people get used to such phenomena as: bitterness in the mouth, heartburn, heaviness in the hypochondrium, unpleasant bloating, constipation, etc. They get used to it and do not perceive these symptoms as a disease. But in fact, these are alarm bells. The body signals, asks for attention.
In order to better navigate the state of your body, you need to have information about the structure and functions of the gastrointestinal tract and, at least, have an idea of the main diseases of the gastrointestinal tract and clearly know the measures for the prevention of gastrointestinal diseases.
Therefore, I conducted introductory lectures and class hours on the structure of the digestive system, symptoms of gastrointestinal diseases and the causes of their occurrence for the students of school No. 12 and the Center for Out-of-School Work. Recommendations for the prevention of gastrointestinal diseases were drawn up and distributed. Information about gastrointestinal diseases is posted in classrooms.
Thus, due to the increase in the incidence of the gastrointestinal tract among children and adolescents, timely and high-quality preventive and dispensary observation, treatment using modern treatment regimens is urgent. Also, routine medical examinations play an important role in identifying various pathologies.
I would like to finish my work with the words of the medieval doctor Arnold from Villanova:
“If you follow your health, you will live a long time in the world.
If there are not enough doctors, let them be your doctors
Three: cheerful character, peace and moderation in food. "
Salerno code of health 1480
Literature
1. Internal Medicine: Textbook /, etc .; ed. , M .: Medicine, 1990.
2., G,. Features of gastroenterological pathology in children and ways to optimize gastroenterological care. // Health of the Russian Federation. –2006. –No. 1.
3. Pediatrics. - M .: Profit-Style, 2006.
4. Indicators of the maternal and child health service in the Bryansk region in 2011.- Bryansk: Medical Information and Analytical Center, 2011.
5. Weight gain of a person. - M: Medicine, 1985.
6. Verse of local immunity in chronic diseases of the gastrointestinal tract. - M .: Medicine, 1999.
7., // Surgery of the digestive tract Kiev: Zdorov'ya, 1987.
8.http: // www. gastroportal /
9.http: // ru. wikipedia. org /
Annex 1
Data of the day hospital of the gastroenterology department
GBUZ "Bryansk City Children's Hospital No. 1"
Distribution by nosological forms
Functional dyspepsia | Gastritis, gastroduodenitis | Peptic ulcer | Dysfunction of the biliary tract | Cholelithiasis | ||
Appendix 2
Clinical examination of children in 2012
Organ diseases digestion | At the beginning of the year | Registered | Received treatment | Withdrawn from the register | At the end of the year |
|
Stomach ulcer and 12 duodenum | ||||||
Gastritis and gastroduodenitis | ||||||
Pancreatitis | ||||||
Gallbladder disease | ||||||
Gallstone disease (gallstone disease) | ||||||
Chronic constipation | ||||||
Total: |
Appendix 3
Clinical examination of adolescents in 2012
Organ diseases digestion | At the beginning of the year | Registered | Received treatment | Withdrawn from the register | At the end of the year |
Peptic ulcer | |||||
Chronic gastritis | |||||
Biliary dyskinesia (BDT) | |||||
Gallstone disease (gallstone disease) | |||||
Total: |
Appendix 4
Application form
1. What diseases of the gastrointestinal tract do you know?
2. Do you have any diseases of the gastrointestinal tract?
3. Are you registered with the dispensary? What is the disease?
4. What foods do your family prefer?
5. What is useful to eat?
6. What foods can you rarely eat?
7. How often do you eat fast food?
8. Do you have bad habits?
9. How do you assess your state of health?
10. What, in your opinion, most of all worsens your health at the present time?
11. What is your age?
12. What is your gender?
Appendix 5
Appendix 6
https://pandia.ru/text/78/051/images/image003_4.png "width =" 616 "height =" 375 id = ">
Appendix 8

Appendix 9
Memo for primary school children:
Eat right!

· Eat meat, butter, milk, bread, cereals, fresh vegetables and fruits every day.
· Eat at least 4 times a day.
· Eating should be done in a calm environment.
· Do not eat before bed.
· Do not snack on chips and crackers.
Chew food thoroughly.
Appendix 10
The structure of the digestive system
Choose the correct answer to the question from the options provided. There may be several correct answers.
1. Typhoid fever refers to:
1. Airborne infections.
2. Quarantine infections.
3. Anthroponoses.
4. Anthropozoonoses.
5. Especially dangerous infections.
2. Antibodies to the causative agent of typhoid fever appear in the blood on:
1.1 week.
2. Week 2.
3.3 week.
4.4 week.
5. 5 weeks.
3. Specify the changes in the mucous membrane of the small intestine in typhoid fever:
1. Diphtheria enteritis.
2. Phlegmonous enteritis.
3. Ulcerative enteritis.
4. Catarrhal enteritis.
5. Purulent enteritis.
4. Give the characteristics of ulcers in the small intestine with typhoid fever:
1. Located across the intestinal tube.
2. Located along the length of the intestine.
3. The edges and shape are uneven.
4. Arise in place of group follicles.
5. The edges are smooth, rounded.
5. Specify the most typical outcome of intestinal ulcers healing in typhoid fever:
1. Small scars.
2. Severe scars.
3. Complete restoration of lymphoid tissue.
4. Lymphoid tissue is not restored.
5. Pigmentation in the area of healed ulcers.
6. Intestinal bleeding, as a complication of typhoid fever, can develop on:
1.1 week.
2. Week 2.
3.3 week.
4.4 week.
5. 5 weeks.
7. Name the extraintestinal complications of typhoid fever:
1. Pneumonia.
2. Purulent perichondritis of the larynx.
3. Amyloidosis.
4. Waxy necrosis of the rectus abdominis muscles.
5. Osteomyelitis.
8. Salmonellosis refers to:
1. Anthropozoonoses.
2. Anthroponoses.
3. Airborne infections.
4. Quarantine infections.
5. Parenteral infections.
9. Name the morphological forms of salmonellosis:
1. Primary.
2. Intestinal.
3. Septic.
4. With the defeat of the mesenteric lymph nodes.
5. Typhoid.
10. Name the most typical complication of typhoid fever:
1. Cicatricial stenosis of the intestine.
2. Amyloidosis.
3. Pyelonephritis.
4. Bowel perforation.
5. Cachexia.
11. Specify the types of intestinal inflammation in the second stage of dysentery:
1. Phlegmonous.
2. Ulcerative.
3. Croupous.
4. Diphtheritic.
5. Catarrhal.
12. Indicate the most frequent localization of pathological changes in dysentery:
1. The jejunum.
3. Sigmoid colon.
4. The ileum.
5. Descending intestine.
13. Give a characteristic of vascular disorders in the intestinal wall with dysentery:
1. Vascular rupture.
2. Full blood.
4. Diapedetic hemorrhage.
5. Thromboembolism.
14. Name the changes in the colon in the third stage of dysentery:
1. Catarrhal colitis.
2. Fibrinous colitis.
3. Ulcerative colitis.
4. Purulent colitis.
5. Serous colitis.
15. List the intestinal complications that can occur with dysentery:
1. Bowel perforation.
3. Amyloidosis.
4. Intestinal phlegmon.
5. Intestinal bleeding.
16. Name the extraintestinal complications of acute dysentery:
1. Bronchopneumonia.
2. Pyelonephritis.
3. Meningitis.
4. Liver abscess.
5. Arthritis.
17. Name the extraintestinal complications of chronic dysentery:
1. Obesity.
2. Cachexia.
3. Pneumonia.
4. Amyloidosis.
5. Myxedema.
18. Give a characteristic of the changes in the mesenteric lymph nodes in the second stage of typhoid fever:
1. The lymphoid tissue is displaced.
2. The size of the lymph nodes is enlarged.
3. The occurrence of typhoid granulomas is possible.
4. Hyperplasia of B-dependent zones.
19. Name the nonspecific complications of cholera:
1. Anemia.
2. Venous congestion.
3. Typhoid.
4. Sepsis.
20. What are the stages of changes in the small intestine with typhoid fever:
1. Brain swelling.
2. Fibrinous enteritis.
3. Purulent enteritis.
4. Stage of necrosis.
5. Stage of pure ulcers.
21. List the intestinal complications arising from typhoid fever:
1. Cicatricial stenosis.
2. Peritonitis.
3. Perforation.
4. Bleeding.
5. Hypermelanosis.
22. Specify the route of infection with typhoid fever:
1. Fecal-oral.
2. Contact.
3. Parenteral.
4. Airborne.
5. Transmissive.
23. Specify the path of penetration of the pathogen into the intestinal wall with typhoid fever:
1. Intraepithelial.
2. Thixotropy.
3. The causative agent is located in the intestinal lumen.
4. Interepithelial.
5. Lymphogenous.
24. Specify the biological environment in which the causative agent of typhoid fever can be found in the first week of the disease:
25. List the forms of typhoid fever, depending on the localization of local changes:
1. Pneumotif.
2. Ileotiff.
3. Ileocolotif.
4. Meningotif.
5. Cholangiotif.
26. Specify the structures of the intestinal wall in which changes develop in typhoid fever:
1. Serous membrane.
2. The muscle layer.
3. Group lymphoid follicles.
4. Nerve plexuses.
5. Solitary follicles.
27. Name the second stage of cholera:
1. Gastroenteritis.
2. Pyelonephritis.
3. Dehydration.
4. Anasarka.
5. Fibrinous colitis.
28. Indicate the changes that are characteristic of the algid period of cholera:
1. Gastroenteritis.
3. Anasarka.
4. Dehydration.
5. Pulmonary edema.
29. Name the clinical and morphological types of dysentery colitis in children:
1. Phlegmonous.
2. Ulcerative.
3. Follicular.
4. Follicular ulcerative.
5. Granulomatous.
30. Morphological changes of the small intestine in the algid period of cholera:
2. Enteritis.
3. Polyps of the mucous membrane.
4. Necrosis of the mucous membrane.
5. Pigmentation of the mucous membrane.
31. Specify the changes in the lymph nodes and spleen in typhoid fever:
1. Amyloidosis.
2. Atrophy.
3. Anemia.
4. Formation of granulomas.
5. Hemosiderosis.
32. Name the causative agent of cholera:
1. Salmonella.
2. Shigella.
3. Vibrion El-Tor.
4. Vibrio Koch.
5. Mycobacterium.
33. Specify the route of infection with cholera:
1. Airborne.
2. Parenteral.
3. Alimentary.
4. Transmissive.
5. Contact.
34. The source of cholera infection is:
1. Sick animal.
2. Sick person.
3. Blood transfused.
4. Vibrio carrier.
5. Household items.
35. Indicate the reservoir (habitat) of Vibrio El-Tor:
1. Sick person.
2. Sick animal.
4. Vibrio carrier.
36. List the periods of cholera:
1. Enteritis.
3. Fibrinous colitis.
4. Ulcerative colitis.
5. Gastroenteritis.
37. Name the parts of the intestine in which the main changes in cholera are localized:
1. The jejunum.
2. The ileum.
3. Sigmoid colon.
4. The transverse colon.
38. Name the changes in the internal organs in cholera during the algid period:
1. Atrophy of the lymphoid tissue of the spleen.
2. Necrosis of the epithelium of the tubules of the kidney.
3. Amyloidosis.
4. Myocardial dystrophy.
5. Purulent meningitis.
39. Name the specific complications of cholera:
1. Amyloidosis.
2. Hyalinosis.
3. Typhoid.
4. Gangrene of the intestine.
5. Uremia.
40. Name a possible complication of alterative changes in lymph nodes in typhoid fever:
1. Gangrene of the intestine.
3. Peritonitis.
4. Myocardial infarction.
5. Amyloidosis.
41. Give the name of the changes in the group follicles of the small intestine in the first stage of typhoid fever:
2. Fibrinous enteritis.
3. Brain swelling.
4. Gangrene of the intestine.
5. Formation of clean ulcers.
42. Name the type of inflammation in the intestinal lymphoid tissue in typhoid fever:
1. Exudative.
2. Fibrinous.
3. Chronic productive.
4. Sharp productive.
5. Purulent.
43. Name the cells that predominate in the group follicles of the small intestine in the first and second stages of typhoid fever:
1. Macrophages.
2. Lymphocytes.
3. Leukocytes.
4. Eosinophils.
5. Giant cells of foreign bodies.
44. The accumulation of macrophages in the intestinal lymphoid tissue in typhoid fever is called:
1. Abscess.
2. Heart attack.
3. Empyema.
4. Granuloma.
5. Phlegmon.
45. Specify the changes in enterocytes characteristic of cholera:
1. Displacement of cell organelles to the apical part.
2. Vacuolation and loss of microvilli.
3. Hyaline droplet dystrophy.
4. Fatty degeneration.
5. Cell proliferation.
46. The pathogenesis of local changes in cholera is:
1. Increased secretion of isotonic fluid.
2. Damage to cell membranes.
3. Lymphostasis.
4. Venous congestion.
5. Violation of liquid suction back.
47. List the nonspecific complications of cholera:
1. Pneumonia.
2. Abscesses.
3. Erysipelas.
4. Amyloidosis.
5. Sepsis.
48. What is the most frequent outcome of the healing of dysentery ulcers:
1. Complete regeneration.
2. Substitution.
3. Formation of rough scars.
4. Malignancy.
5. Hyperplasia of the epithelium.
49. Specify the changes in the small intestine characteristic of 3 weeks of typhoid fever:
1. Venous congestion.
2. Brain swelling.
3. Dirty ulcers.
4. Gangrene.
5. Scarring.
50. The most common complication of typhoid fever is:
1. Hepatitis.
2. Meningitis.
3. Intestinal bleeding.
5. Exhaustion.
51. Indicate the stage of the course of dysentery at which the development of paraproctitis and peritonitis is possible:
1. First.
2. Second.
3. Third.
4. Fourth.
52. Name the causative agent of dysentery:
1. Salmonella.
2. Mycobacterium.
3. Shigella.
4. Cryptococcus.
5. Streptococcus.
53. Specify the path of penetration of the pathogen into the intestinal wall in case of dysentery:
1. Interepithelial.
2. Transepithelial.
3. Intraepithelial.
4. Thixotropy.
5. Chemotaxis.
54. Indicate the main pathogenetic mechanisms of action of the causative agent of dysentery:
1. Cytolytic.
2. Chemotactic.
3. Vasoneuroparalytic.
4. Hypoxic.
5. Lymphotropic.
55. Specify the changes in the intestines that occur during the course of dysentery:
1. Catarrhal colitis.
2. Croupous colitis.
3. Diphtheria colitis.
4. Stage of ulcer healing.
5. Purulent colitis.
56. Indicate the possible intestinal complications that can develop in connection with the regeneration of ulcers in dysentery:
1. Bleeding.
2. Perforation.
3. Peritonitis.
4. Stenosis of the intestinal lumen.
5. Diverticulosis.
57. What are the general changes in dysentery:
1. Hyperplasia of the spleen.
2. Fatty degeneration of the liver.
3. Necrosis of the epithelium of the tubules of the kidney.
4. Metastatic calcification.
5. Fibrosing alveolitis.
58. In case of dysentery, a violation may develop:
1. Fat metabolism.
2. Protein metabolism.
3. Carbohydrate metabolism.
4. Mineral exchange.
59. Macroscopic changes in the spleen in cholera typhoid:
1. Pulp hyperplasia.
2. Greasy sectional view.
3. Pulp atrophy.
4. Heart attacks.
5. Hyalinosis of the capsule.
60. Specify the changes in the colon with cholera typhoid:
1. Atrophy of the mucous membrane.
2. Swelling of the mucous membrane.
3. Purulent colitis.
4. Diphtheria colitis.
5. Croupous colitis.
61. List the possible changes in internal organs in cholera typhoid:
1. Spleen infarction.
2. Foci of liver necrosis.
3. Subacute extracapillary glomerulonephritis.
4. Hyperplasia of the spleen.
5. Amyloidosis of the spleen.
62. List the biological fluids in which the causative agent of typhoid fever is found in the second week of the disease:
1. In the blood.
3. In bile.
5. In the lymph.
63. List the stages of changes in the intestine with typhoid fever:
1. Brain swelling.
2. Necrosis.
3. Formation of ulcers.
4. Stage of dystrophy.
5. Healing.
64. List the general changes in the body, typical for typhoid fever:
1. Exanthema.
2. Hyperplasia of the spleen.
3. Dystrophy of parenchymal organs.
4. Hyalinosis of arterioles.
5. Glomerulonephritis.
65. Macroscopic characteristics of the spleen during the algid period of cholera:
1. Reduced in size.
2. Increased in size.
3. The pulp does not scrape.
4. The pulp gives an abundant scraping.
66. List the pathogenic effect of exotoxin secreted by Shigella:
1. Vasoparalytic.
2. Chemotactic.
3. Lymphotropic.
4. Damages the intramural ganglia.
5. Causes the formation of granulomas.
67. Give a macroscopic characteristic of changes in the intestinal wall in diphtheria colitis:
1. The wall is thinned.
2. The wall is thickened.
3. The mucous membrane is necrotic.
4. Increased blood vessels filling.
5. Anemia.
68. List the possible changes that occur in the lungs with an abdominal type:
1. Bronchitis.
2. Emphysema.
3. Focal pneumonia.
4. Abscess.
5. Croupous pneumonia.
69. List the names of extraintestinal forms of typhoid fever:
1. Meningotif.
2. Pneumotif.
3. Cholangiotif.
4. Sepsis.
5. Cholera typhoid.
70. The accumulation of cells in the lymph nodes, characteristic of typhoid fever, are called:
1. Follicle.
2. Abscess.
3. Granuloma.
4. Sinus histiocytosis.
5. Infiltration.
71. Specify the morphological manifestation of alteration in the lymph nodes in typhoid fever:
1. Granuloma.
2. Abscess.
3. Necrosis.
4. Amyloidosis.
5. Hyalinosis.
72. Specify the possible nature of colitis in dysentery in adults:
1. Gangrenous.
2. Ulcerative.
3. Catarrhal.
4. Follicular.
5. Follicular ulcerative.
73. List the changes in the small intestine with cholera enteritis:
1. Dystrophic changes in the epithelium.
2. Vascular congestion and hemorrhage.
3. Brown atrophy.
4. Swelling of the intestinal wall.
5. Lympho-macrophage infiltration of the stroma.
74. Specify the topographic localization of changes in cholera typhoid:
1. Small intestine.
2. Sigmoid colon.
3. The transverse colon.
4. The cecum.
5. The ileum.
75. Specify the nature of the inflammation in the small intestine in cholera:
1. Productive.
2. Fibrinous.
3. Purulent.
4. Catarrhal.
76. Give the name of the fourth stage of changes in group follicles in typhoid fever:
1. Dirty ulcers.
2. Pure ulcers.
3. Brain swelling.
4. Ulceration.
5. Scarring.
77. Quarantine infections include:
1. Smallpox.
2. Tuberculosis.
4. Yellow fever.
5. Malaria.
78. Specify the duration of the incubation period for cholera:
1. Several hours.
2. 3-5 days.
3. 1-2 months.
4.1-4 weeks.
5. 1-2 weeks.
79. List the mechanisms of action of Vibrio cholerae exotoxin and mucinase enzyme:
1. Secretion of isotonic fluid.
2. Spasm of intestinal smooth muscles.
3. Blockade of the "sodium pump" of cells.
4. Violation of liquid suction back.
5. Damage to cell and vascular membranes.
80. Give a general description of the algid period of cholera:
1. Metabolic acidosis.
2. Hyperergia.
3. Thickening of the blood.
4. Oliguria.
5. Burning of body temperature.
81. List the main reasons for the development of cholera coma:
1. Hypoproteinemia.
2. Progressive exicosis.
3. Hyperlipidemia.
4. Oliguria.
5. Electrolyte imbalance.
82. List the macroscopic changes in the small intestine with cholera enteritis:
1. The intestinal wall is thinned.
2. The mucous membrane is necrotic.
3. The mucous membrane is edematous.
4. Multiple mucosal hemorrhages.
5. Ulceration.
83. Specify the features of rigor mortis in cholera:
1. It is expressed weakly.
2. Disappears quickly.
3. Expressed significantly.
4. It lasts a long time.
5. It is developing rapidly.
84. Microscopic changes in the kidneys with postcholera uremia:
1. Subacute extracapillary glomerulonephritis.
2. Mesangioproliferative glomerulonephritis.
3. Amyloidosis.
4. Infarct-like necrosis of the cortex.
5. Acute pyelonephritis.
85. List the main causes of death of patients during the algid period of cholera:
1. Acute cardiovascular failure.
2. Acute liver failure.
4. Uremia.
5. Intoxication.
86. Specify the duration of the incubation period of typhoid fever:
1. 1-3 months.
2. 2-6 weeks.
3. 10-14 days.
4. 1-2 days.
5.1-5 hours.
87. Give the characteristics of typhoid cells:
1. Refers to macrophages.
2. Refers to lymphocytes.
3. Giant multinucleated cells.
4. Cells with light cytoplasm.
5. The cytoplasm contains the infectious agent.
88. List the organs in which the formation of typhoid granulomas is possible:
1. Lungs.
2. Heart.
3. Lymph nodes.
4. Bone marrow.
89. List the causes of death of patients with typhoid fever:
1. Intra-intestinal bleeding.
2. Peritonitis.
3. Pneumonia.
4. Sepsis.
5. Amyloidosis.
90. Describe the septic form of salmonellosis:
1. Changes in the intestine are significant.
2. Changes in the intestine are poorly expressed.
3. Abscesses in many internal organs.
4. Diphtheria colitis.
5. Catarrhal gastroenterocolitis.
In practice, all registered OCIs are usually divided into three main groups:
- diseases caused by an unknown pathogen (about 70% of cases);
- acute intestinal infections caused by an established pathogen (about 20%);
- bacterial dysentery (about 10%).

The fact that 70% of AEI cases are associated with diseases with an unknown pathogen can be considered a consequence of the “syndromic” principle of diagnosis, which is generally accepted for AEI, which fully justifies itself in diseases that are not epidemic in nature. Indeed, in sporadic AEI (and there are most of them), the similarity of the clinical picture and course of diseases of various etiologies allows not to waste time on accurately identifying the pathogen, since this does not significantly affect the choice of treatment strategy and tactics. In case of epidemic AEI, the earliest possible isolation and identification of the causative agent of the disease, on the contrary, become the most important task, which, unfortunately, requires a significant investment of time and the availability of a well-equipped laboratory.
It is important that the most extensive group of AEI of unknown etiology also includes most of the so-called foodborne toxicoinfections (IPT) - this group is made up of approximately 20 etiologically different, but pathogenetically and clinically similar diseases that do not pose an epidemic danger.
In more than half of the cases, the etiology of AEI cannot be established either clinically or in the laboratory. This task, as well as the choice of pathogenetic treatment, all the more cannot be solved (and is not posed) at the stage of prehospital care. The efforts of the ambulance doctor (EMS) should be aimed at:
- correction of severe disorders of vital functions of the patient's body;
- differentiation of infectious, therapeutic or surgical genesis of the disease;
- solving the issue of the need for hospitalization of the patient for specialized treatment or anti-epidemic measures.
Clinical picture of OCI
AEI - diseases of various etiology and semiotics - combine a common for all these conditions, mainly fecal-oral, method of transmission of the pathogen and the development, as a result of this, of a characteristic symptom complex of acute diarrhea ().
At the same time, the severity of the diarrheal syndrome, as well as the severity of the general condition, the possible outcomes and treatment strategy of the disease are determined by the causative agent of the infection. With all the relativity of syndromic preclinical diagnosis of AEI, it is possible to identify the signs most characteristic of diarrhea of various etiology. Thus, bacterial diarrhea (BD) is distinguished by a more severe clinical course and a more unfavorable prognosis compared to viral diarrhea, since the pathophysiological mechanisms of BD consist in damage to the mucous membrane of the gastrointestinal tract by bacterial enterotoxins or as a result of invasion of microorganisms into epithelial cells. The incubation period for BD can last from 6-8 hours to 7-10 days, but most often it is about 3 days. The shortest incubation period is in coccal infections and salmonellosis. The debut of the DB is accompanied by severe intoxication, a significant deterioration in general health, dehydration, headache, fever up to 38-39 ° C, nausea and vomiting. With the generalization of the infection, symptoms of irritation of the meninges, muscle and bone-joint pain may appear. BD is always accompanied by painful tenesmus and cramping severe abdominal pain, and in dysentery it leads to bloody stools. Often, men with BD develop Reiter's syndrome (arthritis, conjunctivitis, urethritis). In the acute phase of the disease, specific symptoms of one or another DB pathogen are also manifested. The prognosis of BD is always alarming, and with a clinically delineated course of the disease, in all cases, hospitalization and an epidemiological assessment are required.
PTI also belongs to the DB, as it is caused by opportunistic bacteria and in some cases has a group, explosive nature. However, in the overwhelming majority of cases, IPT occurs sporadically with the development of acute gastritis, gastroenteritis or gastroenterocolitis, with varying degrees of dehydration and intoxication, and have a favorable prognosis.
With diarrhea of viral etiology (VD), the integrity of the mucous membrane of the gastrointestinal tract in most cases is not violated and the colon is rarely involved in the process. The incubation period is usually shorter than with epidemic DB. Acute viral gastroenteritis, although accompanied by fever and disruption of the general condition of the patient, rarely leads to severe intoxication, the development of a pronounced inflammatory reaction and dehydration of the patient's body. Significant differential criteria of VD include the absence of severe abdominal pain in these diseases, watery, and not mucopurulent and bloody feces. VD is often accompanied by acute respiratory illness, especially in children. The duration of VD rarely exceeds 3 days, and in general, the disease has a favorable prognosis. Patients with a relatively mild course of VD do not need hospitalization.
In the modern classification of AEI, the so-called special forms of the disease are distinguished:
- travelers' diarrhea;
- diarrhea in homosexual men;
- diarrhea in HIV-infected people;
- antibiotic-associated diarrhea;
- syndrome of bacterial overgrowth in the gastrointestinal tract.
Of the special forms of AEI, only one of the variants of antibiotic-associated diarrhea, pseudomembranous colitis, is important for the practice of an emergency doctor. This disease develops during or significantly after taking antibacterial drugs and is associated with colonization of the intestine by the opportunistic microorganism clostridium difficile. Pseudomembranous colitis proceeds with high fever, bloody diarrhea, abdominal pain and is accompanied by significant intoxication with all possible complications of acute profuse diarrhea. If pseudomembranous colitis is suspected, the patient should be admitted to an infectious diseases hospital.
Preclinical and differential diagnosis of OD
A comprehensive study of the history of the present disease is the first step in the examination of patients with characteristic signs of AEI ().
Patients need to find out:
- when and how the disease began (for example, sudden or gradual development of the disease, the presence of an incubation or prodromal period);
- the nature of the stool (watery, bloody, mixed with mucus or pus, greasy, etc.);
- stool frequency, number and soreness of bowel movements;
- the presence of symptoms of dysentery (fever, tenesmus, blood and / or pus in the stool).
In a conversation with a patient, it is very important to establish the presence and, which is especially important, the development of subjective and objective manifestations of dehydration (thirst, tachycardia, orthostatic reactions, decreased urine output, lethargy and impaired consciousness, seizures, decreased skin turgor) and intoxication (headache, nausea, vomiting, muscle pain).
In addition, in all cases it is necessary to identify possible risk factors for AEI: travel to countries with an epidemic situation that is unfavorable for infectious diarrhea; occupation; recent consumption of unsafe foods (for example, insufficiently cooked meat, raw eggs or shellfish, unpasteurized milk and juices); bathing in polluted bodies of water or using water from them for drinking (for example, water from a lake or river); staying in the countryside, visiting "children's" zoos, contact with wild or domestic animals; presence in the environment of patients with similar symptoms; regular or recent medication (antibiotics, antacids, antidiarrheals); the presence of medical factors predisposing to the development of infectious diarrhea (HIV, taking immunosuppressants, a history of gastrectomy, early childhood or old age); addiction to anal sex; belonging to decreed groups of the population (food workers, educators of children's institutions).
At the prehospital stage, AEI must be differentiated from a number of acute non-infectious diseases of a surgical, therapeutic, gynecological and other profile. The only purpose of differential diagnosis in this case is to choose the direction of hospitalization of the patient. The main criteria for the differential diagnosis are reflected in our proposed prehospital medical care algorithm (Fig. 2).

The prevalence of misdiagnosis of AEI is illustrated by the data of DuPont H. L. (1997). The data provided by the author for the analysis of more than 50 thousand hospitalizations of patients with acute intestinal infections state that in 7.4% of cases this diagnosis was made in diseases such as acute appendicitis, acute cholecystopancreatitis, strangulated intestinal obstruction, mesenteric vascular thrombosis, myocardial infarction, croupous pneumonia, decompensation of diabetes mellitus, hypertensive crisis. On the contrary, the above diseases were misdiagnosed in patients with AEI in 11.1% of cases.
Prehospital therapy for OD
The greatest threat for patients with AEI is the development of dehydration and associated arterial hypotension against the background of intoxication, which provokes a drop in blood pressure and dysfunction of the central nervous system. The scope of prehospital therapy in AEI is based on monitoring the vital functions of the patient's body: the state of consciousness and the function of external respiration, the level of blood pressure and hydration of the patient. In the presence of appropriate equipment for the ambulance team, therapy of clinically significant hypovolemic and infectious-toxic arterial hypotension should be carried out under the control of central venous pressure. In accordance with standard recommendations, therapy at this stage is aimed at:
- to restore the heart rate;
- to optimize the volume of circulating blood;
- to eliminate hypoxia and normalize acid-base balance;
- to carry out inotropic / vasopressor therapy.
To eliminate hypoxia, the patient is prescribed oxygen therapy with a gas mixture with a 35% oxygen content.
Rehydration of the patient begins with the diagnosis of dehydration, the severity of which can vary from I to IV degrees ().
With dehydration of I and II degrees (85-95% of patients with acute intestinal infections), fluid loss can and should be replenished by the oral route. WHO recommends using solutions for oral rehydration with the following recipe: 3.5 g NaCl, 2.5 g NaHCO 3 (or 2.9 g sodium citrate), 1.5 g KCl and 20 g glucose or its polymers (for example, 40 g sucrose , or 4 tablespoons of sugar, or 50-60 g of boiled rice, corn, sorghum, millet, wheat or potatoes) per liter of water. This produces a solution containing approximately 90 mmol Na, 20 mmol K, 80 mmol Cl, 30 mmol HCO3 and 111 mmol glucose. Any of the ready-made oral rehydration solutions (citroglucosalan, rehydron, gastrolit) can be successfully used. The amount of liquid drunk should be 1.5 times higher than its loss with feces and urine. Compensation for dehydration is accompanied by an obvious decrease in thirst, normalization of urine output and improvement in the general condition of the patient.
Dehydration of III and IV degrees, severe nausea or vomiting, as well as unconsciousness of the patient require urgent fluid therapy. For intravenous rehydration, polyionic crystalloid solutions are used: trisol, quartasol, chlosal, acesol. Less effective is the introduction of mono-ionic solutions (saline sodium chloride solution, 5% glucose solution), as well as unbalanced polyionic solutions (Ringer's solution, mafusol, lactasol). Colloidal solutions (hemodez, rheopolyglucin, refortan) are administered only in cases of persistent hypotension, after restoring the volume of circulating blood as a whole. In severe cases, the infusion of water-electrolyte mixtures begins at a volumetric rate of 70-90 ml / min, with an average severity of the patient's condition - at a volumetric rate of 60-80 ml / min. In some cases, the required infusion rate is provided by simultaneous infusion into 2-3 veins. After stabilization of blood pressure, the infusion rate is reduced to 10-20 ml / min. To prevent the progression of dehydration, the development of hemodynamic failure, pulmonary edema, pneumonia, disseminated intravascular coagulation and acute renal failure, the volume of fluid administered after stabilization of the patient's condition may be 50-120 ml per 1 kg of body weight.
Prescribing antibiotic therapy for moderate and severe AEI at the preclinical stage is not only beyond the scope of the EMS doctor, but is categorically contraindicated, since it can significantly worsen the patient's condition and complicate laboratory verification of the causative agent of the disease. The growing threat of infections caused by antibiotic-resistant strains of microorganisms, the presence of adverse reactions when using antimicrobial drugs, superinfection associated with the eradication of normal microflora with antibacterial agents, and the possibility of antibiotic induction of certain virulence factors in enteropathogens (for example, induction of toxinolones of the phage ), are forced to carefully weigh the pros and cons when deciding on antimicrobial therapy and prescribe it only after an accurate diagnosis of the causative agent of AEI. In connection with the foregoing, antibacterial drugs are especially not recommended for gastroenteric variant of OD of any severity, with a mild, erased course of colitis, and during the period of convalescence with any form of intestinal disease.
Empirical prescription of antibiotics is possible in the case of mild and moderate acute intestinal infections of any etiology, as well as in travelers' diarrhea, the most likely causative agent of which is enterotoxigenic strains of E. coli or other bacterial pathogens. In this case, fluoroquinolones are prescribed for adults, and co-trimoxazole for children, the use of which can reduce the duration of the disease from 3-5 to 1-2 days. For this category of patients, who, as a rule, do not need hospitalization, outpatient administration of intestinal antiseptics can be recommended: ercefuril, intetrix or enterosediv in standard doses for 5-7 days, as well as non-antimicrobial drugs that alleviate the course of diarrhea ().
As dangerous as antibiotics, in relation to the aggravation of intoxication is the use of any clinical course of strong antidiarrheal drugs (imodium) and anti-nausea drugs (cerucala, torecan).
Of particular importance in AEI is the correction of intestinal microbiocenosis with probiotics, carried out at various stages of treatment: in the acute period - in order to competitively displace pathogenic microflora, in convalescents - to ensure rehabilitation processes. Very effective early, no later than the second day of illness, the appointment of bifidumbacterin forte in shock doses (50 doses 3 times every 2 hours on the first day of treatment), followed by maintenance doses (30 doses per day, according to indications - up to 6 days).
Probiotic IV generation bifidumbacterin forte provides high local colonization of the intestinal mucosa, elimination of pathogenic and opportunistic microflora. A positive clinical effect in moderate salmonellosis was noted after 1-2 days, in severe salmonellosis and dysentery - by the end of the course. Of the probiotics prepared on the basis of microorganisms of the genus Bacillus, the drug of choice is biosporin, prescribed 2 doses 2-3 times a day for 5-7 days. The drug has a pronounced antibacterial, antitoxic and immunomodulatory effect, induces the synthesis of endogenous interferon, stimulates the activity of blood leukocytes, the synthesis of immunoglobulins. With the predominance of enteric syndrome, enterol, obtained from the Boulardi saccharomyces, is recommended. He is prescribed 250 mg 2 times a day for 5 days. In the period of convalescence, along with traditional pathogenetic agents (stimulants of reparation, general and local immune response), it is advisable to use preparations of the obligate flora, optimally - bifidumbacterin forte, which has a stabilizing effect on intestinal microbiocenosis and homeostatic processes.
Despite the expansion of possibilities for verification of the pathogen and a wide range of methods of etiopathogenetic therapy that have appeared in the arsenal of a doctor over the past 20 years, AEI is still associated with high mortality today. So, according to N.D. Yushchuk, with IPT and salmonellosis, the lethality is about 0.1%, and with dysentery - 1.4%, while the cause of 20% of deaths in bacterial dysentery and 44.4% of deaths in all the rest of the OCI is infectious-toxic shock. The reasons for such a high mortality rate probably lie in an inadequate assessment of the prognosis and severity of the patient's condition with AEI and the failure to provide him, including for reasons of insufficient instrumental, drug and informational support, of emergency care at the prehospital stage. Hopefully, our proposed simple algorithm for prehospital medical care for OD (Fig. 2) will be useful for practicing doctors and their patients.
Literature
- DuPont H. L. // Am. J. Gastroenterol. 1997; 92: 1962-75.
- Kehl K. S., Havens P., Behnke C. E., Acheson D. W. // J. Clin. Microbiol. 1997; 35: 2051-4.
- Lobzin Yu. V., Korvyakova E. R., Litusov N. V., Zakharenko S. M. Modern pharmacotherapy of acute intestinal infections. Center of the HTP BZ of the Ministry of Defense of the Russian Federation.
- Mc Qbaid K. R. Diarrhea. Current medical diagnosis and treatment. 38th ed. Appleton & Lange, 1999, p. 546.
- Springs D. et al. Emergency therapy. Geotar, Medicine, 2000.S. 30.
- Yushchuk ND, Brodov LE Principles of diagnosis and treatment of acute intestinal infections // Treating Doctor. 1999. No. 7.P. 40.
Table 1. Typical clinical manifestations of AEI
- Acute profuse diarrhea
- Dehydration
- Intoxication
- Abdominal pain
- Fever
- Admixture of blood in stool