So, the pregnancy is coming to an end, the eighth month has already passed and, finally, the 35th week of pregnancy has come. Pressure is, unfortunately, a fairly common problem that pregnant women often face. The pressure can be both high and low, the problems associated with it can also be of different origin.
Low blood pressure in pregnant women happens quite often and does not have a very good effect on both the woman and the child at any stage of pregnancy. The fact is that with reduced pressure, a woman often feels unwell, weak and dizzy, which has a bad effect on her well-being and mood (in fact, what kind of mood is there if you feel dizzy?). In addition, with reduced pressure, blood flow to the placenta weakens, as a result, the child lacks oxygen and nutrients. In especially severe cases, a woman with very low blood pressure may be hospitalized at any stage of pregnancy. So, pressure below 100/60 is already a sufficient signal to see a doctor, even in itself, without dizziness and other "pleasant" symptoms.
High blood pressure in pregnant women is even more common. Strictly speaking, the second half of pregnancy is an occasion to monitor the pressure even more strictly than before. The fact is that high pressure in pregnant women, it can serve as a very dangerous symptom and be a sign of preeclampsia - a dangerous complication, which, in severe forms, can threaten the health and even the life of both mother and baby.
So, why does blood pressure often rise at the end of pregnancy? In part, this happens for quite natural reasons. An additional circle of blood circulation appears in the body of a pregnant woman, and the volume of blood increases - and quite significantly, by a liter and a half (depending on how much it weighs future mom) . And such an additional volume of blood is not just extra fluid, it is also an additional burden on the heart, which is not so easy to pump such a volume. As a result, the pressure increases slightly. If the difference compared to the "on duty" pressure is small, there is nothing to worry about.
It is quite another matter if a pregnant woman has edema. When edema occurs, fluid accumulates in the tissues, while the volume of blood decreases, it thickens. Yes, and it is much more difficult to penetrate into a swollen, for example, placenta. What happens in this case? And this is what happens: the body launches a kind of protective reaction in order to be able to supply thickened blood to the tissues, while the pressure rises. This situation is very dangerous, because, among other things, thick blood provokes the occurrence of even greater edema. In especially severe cases, a pregnant woman requires urgent hospitalization so that the situation does not get out of control.
When measuring pressure, it is important to distinguish between values that are normal for most people and pressure that is normal for a particular person. So, for most people, the pressure of 120/80 is considered normal, but if in this pregnant woman it has never risen above 110/65, such numbers can indicate alarming symptoms.
High blood pressure in pregnant women is no joke. If the pressure is still elevated, you should definitely consult a doctor and strictly follow his recommendations, even if you feel generally good. If high blood pressure is accompanied by poor tests (for example, protein is found in the urine), feeling unwell(the first thing that is alarming is a sharply worsened state of health and severe fatigue), other symptoms, there is nothing to talk about - you should immediately consult a doctor.
What to drink for pregnant women with pressure: first of all, it is worth noting that at the end of pregnancy it is better to limit as much as possible strong tea and coffee, tonic drinks, sweet carbonated drinks - all this is not only unhealthy for the baby, but also adds a completely unnecessary load on the blood vessels. Best to drink plain water, in small portions, or healthy drinks that quench thirst well (rosehip infusion, cranberry juice, juices). Some juices, other than providing vitamins and other useful substances can help with high blood pressure. For example, cranberry juice is very useful, but you should not cook it for too long, so as not to kill all the vitamins. Birch sap (of course, fresh) is also useful, as well as a decoction of pumpkin with honey. Can help and beetroot juice(its sharp taste may not be liked, in which case it can be mixed with carrot juice) . In order for juices to bring maximum benefit, you need to drink them about half an hour before meals.
If a pregnant woman has high blood pressure, her well-being should be carefully monitored, and the pressure should be measured at least once a day. When measuring pressure, you need to sit, relax (do not cross your legs!), Do not speak or take convulsive breaths.
So, the pregnant woman has a little high blood pressure. What to do: in order for the blood exchange, and hence the pressure, to be normal, it is very important to move for a sufficient amount of time, as well as to rest. On the later dates pregnancy is to walk more, at your own pace, not too fast. Of course, shoes should be comfortable and without heels, stable. In summer, in extreme heat, it is worth postponing a walk until the evening or moving it to the early morning.
In addition, it is highly recommended to sit less in one position, and lie more relaxed, or walk. For the prevention of edema, it is also recommended to take a posture that unloads the kidneys several times a day, this will also alleviate the condition.
Increased or reduced pressure can be obtained with excellent health (and this is not a broken tonometer). Here's what can affect the result: a cup of strong tea or coffee, drunk shortly before measuring pressure, licorice root, anxiety (enough to be nervous about the same visit to the doctor!), as well. . . lying position.
Problems with pressure, swelling and overweight can make life difficult in the later stages of pregnancy, but it is worth remembering that all this is solvable, all problems will pass, and most importantly, with proper care and treatment, you can get rid of them quickly enough.
35 weeks pregnant is already a very long time. This is 8 calendar months and almost 9 obstetric. Most women are already preparing for the upcoming birth. The kid, even if unconsciously, does the same. What changes in the organisms of mother and child occur these days? What signs show that everything is going well, and when should you urgently go to the hospital? What is the optimal daily routine for this period?
Child development
The 35th week of pregnancy is the period when the fetus is already almost formed. There are only a few touches left - and he will be completely ready for life outside his mother's body. A child who was born at 8 months (calendar) usually quickly adapts to a new environment.
Here are some characteristics of the changes that occur during this period:
- Since this week, the weight gain is 200-220 g, the weight is currently 2400-2600 g. But the baby weighs a little more or less, do not worry too much, because each child is individual and has its own set of genes. If one of the parents weighs little or even both, most likely the baby will be miniature.
- The body length of the fetus is 45–47 cm.
- All organ systems are already fully formed, but some are not yet quite ready to work on their own.
- At 35 weeks, the fluff on the body of the fetus disappears.
- Active accumulation of subcutaneous fat begins. Shoulders, arms, legs become childishly rounded. Cheeks appear, skin folds are visible.
- The skin color is already almost the same as that of a normal newborn baby. Its surface is not as wrinkled as before.
- The nails have grown. They have already reached the ends of the fingers, they even protrude a little, so some babies even manage to scratch themselves with them.
- The color of the eyes at this time is blue, no matter what it will be later.
- Movement became less active due to the fact that free space is getting smaller. They are more like rollovers than somersaults like the previous weeks.
- Often it is at this time that the fetus occupies the position in which it will be during childbirth. But if this does not happen, you should not worry very much - some children turn over correctly just a few days before birth.
All these changes can be seen on the ultrasound, which should be done this week.
Ultrasound at 35 weeks
To assess how correctly and timely the development of the child is, whether it corresponds to the gestational age, an ultrasound scan is performed. Ultrasound diagnosis at 35 weeks also helps to make a decision, or at least make an assumption about the tactics of childbirth.
What can you find out during an ultrasound at 35 weeks of gestation? The following data:
- Height, approximate weight, gender of the baby, its location in the uterus.
- Make a conclusion about the absence or presence of malformations.
- The position of the placenta and the degree of its maturity and functionality.
- Condition and amount of amniotic fluid.
- Location and condition of the umbilical cord.
- Correspondence of the size of the pelvis and the head of the fetus.
- The activity of the child, how many times he moves in a certain period of time.
- The correctness of the rhythm of the fetal heart.
After this ultrasound, the doctor may recommend a caesarean section if he notices that there may be difficulties with conventional childbirth. This decision is yours to make. But it is worth remembering that this operation is not so terrible, but in some situations it saves the life of both the child and the mother.
Mom's well-being
By week 35, the abdomen is already very noticeable, the skin is taut, which can cause itching (you can use special creams to increase the elasticity of the abdominal skin), the navel is convex. It may seem to a woman that she is big and clumsy, weighs a lot. Weight from the beginning of pregnancy should normally increase by about 13 kg. You need to make sure that the weight gain is not too large, as this can complicate the process of childbirth.
When the 35th obstetric week begins, many women complain of severe shortness of breath, nausea, almost constant heartburn, and swelling. This is due to the fact that the stomach presses on the internal organs. Nausea, heartburn, vomiting can be observed after a heavy meal, a sharp change in body position, which greatly limits the woman. Also, back pain is often due to a strong load on the spine.
Heartburn can be especially annoying. Almost all pregnant women complain about the presence of this unpleasant phenomenon. Why does heartburn occur? The cause of the symptom is squeezing of the stomach and weakening of the smooth muscles. Because of this, the contents of the stomach easily enter the esophagus. What is felt at the same time is called heartburn.
By the end of the week, the stomach will drop, heartburn and nausea may stop bothering you, but the pressure on the bladder will increase. Now the expectant mother will need to go to the toilet often, which may even develop insomnia.
The sudden appearance of symptoms such as nausea and vomiting, especially with severe edema, may be a sign of late toxicosis. In this case, it does not hurt to go to the hospital and pass the necessary tests, for example, for the presence of protein in the urine.
Motor mode and nutrition

In order not to suffer from nausea, vomiting and heartburn, you need to eat often, but in small portions. The diet should be similar to a child's: rich in vitamins, with dairy products, without fried, salty, spicy and foods that can cause allergies. It is advisable to reduce the consumption of salt, coffee, strong tea. You also need to monitor how much the expectant mother weighs, and if weight gain occurs too quickly, exclude high-calorie foods (buns, pies, sweets). With such a diet, heartburn is observed a little less often.
Heavy physical activity, especially heavy lifting, is strictly prohibited. But lack of movement is also bad for bones and joints. It can also aggravate swelling. Therefore, you need to walk a little, and often change your posture when resting. It is best to sleep on the left side.
Allocations
Discharge at the 35th week of pregnancy is one of the most important indicators by which one can judge how correctly metabolic processes are taking place, whether the expectant mother is healthy, and how soon labor will begin.
Possible selection options and what they say:
- White or transparent, odorless, in moderation - the norm.
- Mucous membranes are also the norm, but indicate that the mucous plug is moving away.
- White, cheesy, accompanied by itching, redness - thrush. It is often aggravated in pregnant women, but it needs to be urgently cured so that by the time of birth the birth canal is clean.
- With bad smell, with a green or brown tint indicate the presence of some kind of infection. You need to see a doctor urgently.
- Bloody discharge, especially if it hurts in the lower abdomen, is a sign of premature placental abruption. This is a direct indication for hospitalization and caesarean section.
- Abundant watery - amniotic fluid departs. Emergency medical intervention is needed.
As you can see, any changes in the nature of the discharge may indicate a serious pathology, the consequences of which, without treatment, can become deplorable. Therefore, in no case do not ignore such signs.
Sex at 35 weeks

In most cases, in late pregnancy, women are not very interested in the question of whether sex is allowed in their position. But if the expectant mother feels well enough, and there are no contraindications, sex at the 35th week of pregnancy is not prohibited.
It used to be thought that uterine contractions during orgasm could trigger preterm labor, but modern medicine does not confirm this fact. On the contrary, studies show that sperm increases the elasticity of the cervix, which is positive for a woman who will soon give birth.
Possible contraindications:
- An ultrasound revealed a multiple pregnancy.
- The threat of premature birth.
- Physical or psychological discomfort, soreness.
- The presence of a sexually transmitted infection or other sexually transmitted infections in a partner.
- The process of expulsion of the mucous plug. As soon as it is discharged, the child becomes open to external infections, even those that may be safe and invisible to parents.
Doctors advise against using condoms, as this can disrupt the microflora, and avoid positions in which pressure is applied to the stomach.
Twin pregnancy - features
If pregnancy is joy, then pregnancy with twins is doubly joy. True, this option has its own characteristics and difficulties, because it is much more difficult for the body to ensure the vital activity of two children.
Consider how the 35th week differs during pregnancy with twins:
- Babies are usually slightly smaller in terms of height and weight than their "peers" who are born alone. Their normal weight is 2100–2500 g.
- The last weeks are even harder for a woman, as her internal organs are squeezed. Even more often than normal pregnancy, nausea, shortness of breath, heartburn, swelling in the legs by the end of the day, back pain. But by the end of the week, the woman will definitely feel how her stomach drops and most of these unpleasant symptoms will pass.
- Very often, childbirth occurs earlier by a couple of weeks. Therefore, if you are expecting two children, by week 35 everything you need to enter the maternity hospital should be completely ready. Doctors advise to go to the hospital at 36-37 weeks, even if it does not look like labor will begin soon.
Childbirth at 35 weeks

Delivery at 34–35 weeks is not normal, but is usually relatively well tolerated by the baby. At this time, the most important organ systems have already formed, so he will be able to breathe on his own and develop no worse than other children. Of course, some problems may arise, for example, in the early days the baby may experience digestive problems and associated weight loss, but this does not have a big impact on further growth and development.
Delivery this week is not uncommon. Therefore, a woman needs to be careful not to miss the symptoms when she needs to call a doctor. But it is worth remembering that contractions can be training, in order to talk about the onset of childbirth, other signs are needed.
Childbirth at 35 weeks of gestation may begin with the following symptoms:
- It hurts a lot in the lower abdomen, contractions occur. Compared to training, they are much more pronounced, repeated more often, and their duration gradually increases.
- The mucous plug comes off. In some cases, it departs gradually, over several weeks. But a variant is possible when everything happens very quickly and childbirth occurs in the near future.
- The amniotic fluid has broken. If it is excreted from the vagina a large number of liquids, you should immediately call a doctor. Even if the birth does not start on its own, the pregnancy cannot be continued, because without amniotic fluid, the baby can suffocate. The doctor will decide to either induce labor or perform a caesarean section.
- The fact that childbirth is approaching at the 35th week of pregnancy can also be indicated by the fact that at the same time as the contractions, the woman is very sick and vomiting occurs.
- There is a feeling that the stomach turns to stone. At the same time, it has already fallen, compared with the situation in previous weeks.
When is a caesarean section necessary?

A caesarean section is prescribed in cases where there is a considerable likelihood that complications will arise during normal childbirth, the consequences of which can be dangerous for a woman or baby.
Indications for surgery:
- Prolapse of the umbilical cord. The umbilical cord delivers oxygen and nutrients to the fetus. When it falls out, it is clamped, and access to nutrition and breathing is blocked. Emergency intervention is necessary so that the fetus does not die.
- Placenta previa or malposition. This is a fairly common pathology early dates. The placenta is attached in such a way that it partially or completely blocks the exit from the uterus. Often, before the start, she takes a safe position, but if this does not happen, normal childbirth becomes impossible. To track the position of the placenta, it is important to do an ultrasound in a timely manner.
- Placental abruption occurs. After placental abruption, life in the abdomen becomes impossible, so a caesarean section is performed.
- Transverse position of the fetus. If childbirth begins, and the child lies incorrectly, it is removed surgically.
- Umbilical cord wrap. If the baby is entangled in the umbilical cord, strangulation may occur during passage through the birth canal. The location of the fetus and umbilical cord is easiest to determine using ultrasound, so it is mandatory to conduct it before childbirth.
- Mismatch between the size of the fetal head and the woman's pelvis. This can also be judged by the results of ultrasound. In most cases, even if the fetal head is large, but it is correctly positioned, childbirth should take place without a threat to life. But they will last a very long time, the risk of complications and ruptures in the birth canal will increase. Therefore, in this case, it is safer to do a caesarean section.
Be attentive to your well-being healthy lifestyle life, cooperate with doctors, regularly do ultrasound and do not doubt that your baby will be fine!
The appearance of my baby began with a three-day sleep deprivation at night, then it turned out to be due to high blood pressure, for three days she walked angry and irritable on the third day, her husband made me measure the pressure by 160 to 90, I didn’t even believe it because I felt fine and the whole pregnancy went with low blood pressure and then there are such numbers, here I have a panic, we call an ambulance, they take me to the hospital, they knocked down the pressure for 2 days, the tests were bad, then they decided to have a cesarean to save the child, and I so wanted to give birth myself, well, that's okay, they began to inject the epidural, they just put me in and told me to bend I lost consciousness on my back from the fact that my pressure was still brought down, they cut me up, they got the baby, he started crying, they didn’t really show me while they sewed me up, the pediatrist comes and says the boy is 2450 grams 44 cm while breathing here I started crying, they brought me to the ward I was trembling after the norcosis, come on to inject with sedatives, I turned off, in the morning the pediatrist comes and says the child is breathing with shortness of breath and I feel something is not right I call my husband so that he calls the maternity hospital and asks everything about the child himself, then hell began, it turned out that the child does not have the strength to breathe, oxygen is not supplied urgently, we need to find a place for the child in intensive care in another hospital, there are no places, they say to wait a day and a day with us it wasn’t that we had to find one single place for my baby to be taken and taken to the hospital, they only showed it to me from afar, I was left alone in the maternity hospital, and such an emptiness of the child didn’t really see the birth, I didn’t have normal lying down and thinking about giving birth whether it was so horrid, really howled in the bed, they didn’t know how to calm me down, they injected me with sedatives, and the doctors persuaded me. They nursed the child for a week in intensive care, then they discharged me and I already lay down with him in a separate bed, then my soul calmed down a little bit. but this is equipment which was connected to him drove me crazy, she periodically sang that the child was not breathing. After 3 weeks, we are only at home, but everything does not stop for me postpartum depression thank you husband and my mom help me. Forgive me for the mistakes for the text is not literate, I still have not come to my senses.

Ekaterina Osochenko, perinatal yoga instructor, mother of six: “You can never be sure in advance whether childbirth will be easy or difficult. However, when a woman knows that her mother brought her into the world herself, without drugs and without any medical intervention, she has the best prognosis. These factors are more important than age, the size of her pelvis, and so on.” These words belong to the world famous obstetrician Michel Auden. At the very beginning of his medical practice in the 60s of the last century, he performed a large number of caesarean sections. At that time, the operation in the lower uterine segment seemed to many doctors to be “miraculous” and “saving”, since it was performed in really complicated births in about 1% of cases. But over the past half century, caesarean sections have become incredibly popular: in many countries, “more than 50% of children are born through this,” Auden writes in his book “Caesarean section: a safe exit or a threat to the future?” in 2004. According to his estimates, in Russia this figure does not yet exceed 15%.
Why did this happen? The fact is that recently the list of relative indications for this operation has “imperceptibly” expanded. Relative indications for caesarean section- These are situations in which natural childbirth is physically possible, but is associated with some risk:
- Large fetus (with sufficient mobility and normal size of the pelvis of the woman in labor, childbirth is possible through the natural birth canal). It is worth remembering that the weight of the child depends on how the mother eats and how much she moves during pregnancy.
- Myopia. By itself, it is not an indication for caesarean section, but changes in the vessels of the fundus are a risk factor, as it can lead to hemorrhage and retinal detachment. Or it may not lead if you teach the woman in labor to push properly, directing the effort not “to the head”, but down.
- Previous caesarean, the presence of one or more scars on the uterus. This is far from absolute! With a wealthy uterine scar, nothing interferes with natural childbirth: up to 20% of women in the world successfully give birth naturally after a previous cesarean.
- Age over 35, which is often considered a relative indication. It is dangerous, of course, not by the number of years lived, but by the state of health. On the other hand, a young and healthy 35-year-old body is not an indication for surgery, but a severe heart defect can be an indication for caesarean section at 18 years of age.
- Lack of oxygen in a child (hypoxia) also refers to relative indications and can be diagnosed no earlier than directly in childbirth using the CTG apparatus. However, overdiagnosis often takes place here: “With the beginning of the widespread use of CTG in childbirth - and this happened during my practice - the percentage of caesarean sections increased as a result of overdiagnosis, but the improvement in the health of newborns in the general mass (as expected) did not happen as a result of this ! I want to remind you: a healthy mother is a healthy baby. If the mother’s cardiovascular system is trained, then there are no problems with the supply of oxygen to the child - neither during childbirth, nor during pregnancy, ”says an obstetrician-gynecologist with 40 years of experience, a specialist in ultrasound diagnostics Tatyana Malysheva.
- Not correct position a baby in the uterus: breech presentation (breech or foot), transverse position, tilting of the head, and so on. They occur in 3.5-6% of cases. Classical medical textbooks on obstetrics describe techniques that allow you to take birth even with the child in the wrong position.
Absolute indications for caesarean section, in which childbirth through the natural birth canal is physically impossible:
- Anatomically narrow pelvis - a condition in which the presenting part of the child cannot pass through the mother's pelvic ring. Diagnosed directly in childbirth!
- Neoplasms (myoma) or complete placenta previa - when the cervix is completely blocked; this condition is diagnosed in advance, in late pregnancy with the help of ultrasound.
- Premature placental abruption - the onset of bleeding, when the fetus has not yet come out, and the birth is not completed. This diagnosis is literally a fraction of a percent among all women in labor, and you do not need to tune in to such an outcome in advance. If the birth takes place in a hospital, the situation has a favorable outcome.
- Threatened uterine rupture. This situation, like the previous one, is extremely rare and is diagnosed only directly in childbirth. Before their onset, it is impossible to predict it. Predisposing factors are multiple pre-pregnancy abortions, and sometimes a scar from a previous caesarean. “The divergence of the scar, as well as the threatening rupture of the unoperated uterus, is extremely rare,” says the obstetrician. Tatyana Malysheva. – For 20 years of work at the ultrasound machine, I was convinced that it is impossible to determine the condition of the scar by ultrasound in advance! You can understand that the divergence of the scar has begun, according to the clinical picture directly in childbirth.
Summing up, I will quote the words again Michel Auden: “Unfortunately, the medical department has captured some episodes of sexual life ... One could say that the obsession with management characterizes all midwifery ... We must reconsider the foundations of midwifery. Our first goal would be to help women make the best use of their own physiological potential. A woman in labor needs intimacy - any interference with her privacy inhibits childbirth.
How is it inside?
At 35 weeks, the baby's heart beats 120-160 times per minute. As a rule, by this time, most babies prefer to turn around "facing the exit", that is, they are in the head presentation. However, the final position of the fetus cannot be judged until childbirth, since at any moment it can turn over.
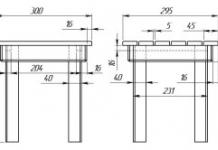
Illustration: Mirta Groffman

There are more and more reasons for this operation every year. We will consider those that are most common: we will decipher the diagnoses and tell you what to prepare for ...
Doctors conditionally divide all indications for caesarean section into two groups: absolute and relative. At 35 weeks pregnant, you already need to know the options!
The first involves cases where the question of whether to operate or not is not discussed. These are such as prolapse of the umbilical cord, placenta previa or abruption, the transverse position of the fetus. We need to save the life of a child and a woman!
The second group is formed by situations (uterine scar, breech presentation, large fetus, high myopia, narrow pelvis, and others), when there is a possibility of natural childbirth. The final decision on the advisability of a caesarean section is made by doctors after studying all the factors. We get acquainted with the main indications for surgery.
1. Placenta previa
Does the expectant mother in the last months of pregnancy have red blood discharge from the genital tract at night? The symptom usually points to placenta previa. If it partially or completely covers the cervix, it makes it difficult or impossible for the child to exit. Full presentation is an absolute indication for a caesarean section. Attention! Such a diagnosis is made only at the end of pregnancy!
After all, expectant mothers who have time left before childbirth are more likely to raise the placenta, which means there is a chance that it will take a completely safe position. Natural childbirth becomes possible!
2. Premature placental abruption
Some pregnant women experience severe abdominal pain. Is it constant, does not stop even for a minute, is it sometimes accompanied by bleeding? All these are true signs of premature detachment of the placenta (complete or partial). The child's life is in danger! Usually, doctors perform immediate operative delivery, since placental abruption is one of the main causes of intrauterine death of a child.

3. Failure of the scar
An absolute indication for caesarean section is the failure of the scar that remained on the woman's uterus after the operation performed earlier. In normal physiological childbirth, there is a threat of uterine rupture!
What scar is called insolvent? Its thickness is less than 3 mm, the contours are uneven, there are inclusions of connective tissue (determined using a detailed ultrasound examination). If there is a suspicion of inferiority of the scar, the pregnant woman should be hospitalized in the maternity hospital long before the birth (at 34-35 weeks).
She will be monitored there. Depending on the condition of the scar, the doctor will determine how the baby will be born.
4. Narrow pelvis
More correctly, from a medical point of view, this indication sounds like this: a discrepancy between the size of the pelvis and the head of the fetus. When the doctor sees that the baby's head is too big to fit through the woman's pelvic bones, he is inclined to perform a caesarean section. But some doctors take risks and allow a future mother with a narrow pelvis to give birth naturally.
They are guided by the fact that often the discrepancy is not obvious, because a lot depends on the location of the baby’s head and how it “configures” during childbirth. Although it must be admitted: such childbirth lasts much longer than usual
5. Cord prolapse
It happens that with the outflow of amniotic fluid (spontaneous or after artificial opening of the fetal bladder), the umbilical cord loop falls through the cervix into the vagina and is outside. It is very dangerous! In this position, the umbilical cord is compressed, which means that the blood stops flowing to the baby. An urgent operation is needed! True, if the birth is in the second stage and the child is about to be born, no one will operate.
It is worth noting that if the fetus is in cephalic presentation, prolapse of the umbilical cord occurs very rarely. What can not be said about the foot presentation of the baby and the premature birth. In such cases, the doctor makes a decision based on the condition of the patient and the baby.
The period of pregnancy is a time of special condition female body when all organs and systems work with increased load. High blood pressure during pregnancy, most often, is the result of a woman's lack of compensatory capabilities. The cardiovascular system during pregnancy is subjected to increased stress: the heart works "for two", the volume of circulating blood increases.
In the normal course of pregnancy, hypertension is not observed, on the contrary, there is a slight decrease blood pressure. This happens under the influence of hormonal substances.
That is, some factors contribute to an increase in pressure, others - to a decrease. An imbalance of these factors causes high blood pressure during pregnancy. Arterial hypertension in pregnant women is diagnosed when the indicator exceeds 140/90 mm. rt. Art.
This limit is not an unambiguous criterion: in women who are hypotensive in everyday life, hypertension can develop with blood pressure, the values of which are within the normal range for other people. Therefore, it is important that every woman knows her usual, normal blood pressure.
Women who had high blood pressure before pregnancy need to carry out a competent correction of hypertension at the planning stage, with the selection of drugs that can be taken during pregnancy. If pregnancy occurs against the background of high blood pressure, an urgent selection of antihypertensive drugs is necessary, otherwise there will be a threat of abortion and serious complications from the mother and child. Arterial hypertension, complicated by vascular pathology, which has a crisis course, is an indication for termination of pregnancy at any time for medical (threat to the life of the mother) indications.
High blood pressure during pregnancy for more than 20 weeks, combined with edema and protein excretion in the urine (proteinuria) should be the object of close attention of an obstetrician-gynecologist. Such a condition that exists for a long time without correction inevitably leads to the development of a formidable complication of pregnancy - preeclampsia. The above symptoms are accompanied by neurological symptoms: headache, dizziness, mental disorders, possibly convulsions, visual disturbances. Preeclampsia is a condition that is dangerous not only for the course of pregnancy, but also for the life of the mother and child.
Why is high blood pressure so dangerous during pregnancy?
The fact is that with increased blood pressure, a compensatory spasm of blood vessels occurs, including the vessels of the uterus with the placenta. As a result, the supply of oxygen to the fetus decreases (sometimes to a critical minimum) and nutrients. The development and growth of the child slows down, while the risk of developing congenital pathologies and various neurological disorders increases in parallel. A decrease in blood supply can also lead to premature detachment of the placenta, accompanied by heavy bleeding.
In order to timely detect an increase in blood pressure during pregnancy and assess the possible development of preeclampsia, at each visit to the gynecologist, blood pressure is measured, weighed (rapid weight gain speaks in favor of edema, possibly hidden), and protein in the urine is determined.
Treatment at the initial stages is carried out by non-drug methods: diet, drinking regimen, physiotherapy. If there is no effect, the woman is usually hospitalized in a hospital for the selection of antihypertensive therapy and monitoring the course of pregnancy.
Blood flow indicators are very important when carrying a baby. Through the blood, the child in the mother's tummy receives all the components it needs for growth. Changes in blood pressure late pregnancy can be very dangerous.

Features in this period
Blood pressure (BP) should be monitored throughout pregnancy. The importance of measuring this indicator of blood flow in the later stages of bearing a baby cannot be overestimated. A change in blood pressure may indicate various pathologies in both the expectant mother and her baby.
Quite often, blood pressure indicators change during pregnancy. This change is largely driven by changing hormonal levels.
Specific pregnancy hormones have a pronounced effect on systemic blood flow. Changes in the lumen of blood vessels under the influence of various hormones lead to an increase or decrease in blood pressure.

Norms
In late pregnancy, it is very important to control blood pressure in the expectant mother. She can do this on her own or with a doctor.
It is better if such measurements are carried out regularly. It is especially important to follow this recommendation for expectant mothers who have problems with blood pressure. Women who are at high risk should also not avoid this simple and routine procedure.

Specialists distinguish several types of AD:
- The first one they call "upper" or systolic. It is determined when the first heartbeat appears when measuring blood pressure using a tonometer. In pregnant women, the systolic pressure should not exceed 140 mm. rt. Art. Its drop is below 100mm. rt. Art. is also an unfavorable sign requiring a visit to a doctor.
- The second type of blood pressure is called diastolic or "lower". Its value corresponds to the last audible heart beat when measuring blood pressure with a tonometer. An increase in this indicator above 100 mm. rt. Art. - an unfavorable sign that requires mandatory consultation with a doctor. It is also necessary to consult a doctor if the diastolic pressure has fallen below 60 mm. rt. Art.
The most optimal pressure that occurs in most women in late pregnancy is 130 to 80 mm. rt. Art. Such figures are not a manifestation of pathology and indicate a normal level of blood flow.

Reasons for change
The stronger the health of the expectant mother before pregnancy, the lower the risk of developing various pathologies in her. Quite a lot of different chronic diseases of internal organs contribute to changes in blood pressure.
In the last stages of pregnancy, pathologies that occur both in the maternal body and on the part of the fetus can lead to jumps in blood pressure. The severity of functional impairment largely depends on how severe the disease is.
According to statistics, high blood pressure is most common in women over 40 years of age. This leads to age-related changes tone and diameter of blood vessels.

If a pregnant woman in the family has one of her close relatives who had hypertension or myocardial infarction, then the risk of developing a persistent increase in blood pressure in her increases several times.
Diseases of cardio-vascular system can also lead to frequent spikes in blood pressure in late pregnancy. Expectant mothers with arrhythmias or other cardiac arrhythmias must additionally visit a cardiologist when carrying a baby.
If they used any cardiac medications before pregnancy, then after conception, you should definitely discuss with your doctor the possibility of their further intake. In such a situation, it may be necessary to cancel some drugs and select new drugs that do not adversely affect the developing fetus.

Expectant mothers who are obese or who have a pronounced excess body weight are also at risk for the development of a persistent increase in blood pressure. It must be remembered that during pregnancy, the load on the female body increases many times over.
The increase in body weight of the baby already entails changes in peripheral blood flow. If a woman's body weight is significantly higher than normal values due to obesity, this will inevitably lead to the fact that when measuring blood pressure, she will receive high values.

Diseases of the kidneys and urinary tract are common causes of hypertension. It is important to note that some of these pathologies are accompanied not by an increase, but by a decrease in blood pressure.
Violation of the outflow of urine leads to a change in the volume of circulating blood in the body. Ultimately, the functional disorders that have arisen are manifested by a change in blood pressure numbers. Quite often, pathologies appear at 35-38 weeks of pregnancy.

Neurological diseases that arose even before the conception of a baby can also have an adverse effect on blood pressure indicators. Various craniocerebral injuries, previously transferred meningitis or meningoencephalitis lead to a persistent change in this indicator of blood flow. In such a situation, the expectant mother You should definitely see a neurologist. This specialist will select the necessary therapy and offer her a number of necessary recommendations.
There are a number of certain pathologies that occur only in pregnant women. One of them is gestosis.
This pathology can be very dangerous for both the mother and her baby. It is accompanied by the development of a persistent change in blood pressure, as well as the appearance of protein in the urinary sediment. General state expectant mother with this pathology is significantly disturbed.

How is it determined?
Persistent deviations from the norm are accompanied by the appearance of adverse symptoms. So, with an increase in blood pressure, a woman develops a headache. The nature of the pain syndrome can be growing and arching.
The pain spreads throughout the head. Usually, epicenter of pain syndrome - on the back of the head. Many women feel a strong pulsation in the temples.
Dizziness is another common symptom that occurs with blood pressure disorders. This clinical sign manifests itself mainly with a change in body position. For many women, dizziness becomes very severe. The severity of the condition can be aggravated by the appearance of "flies" before the eyes.


Expectant mothers who have problems with blood pressure begin to experience rapid fatigue. Even after performing normal daily procedures, they get tired very quickly. To improve their overall well-being in this case, they need to rest more often. Quite often, this symptom appears already in the last weeks of pregnancy.
A common complaint that therapists from pregnant women hear at a doctor's appointment is general weakness. This is a completely normal symptom that occurs at 37-39 weeks of pregnancy. In some cases, it manifests itself much earlier - by 30-32 weeks.


Expectant mothers carrying twins or triplets may be a little more tired. However, in pregnant women who have problems with blood pressure, general weakness can be very pronounced.
This unfavorable symptom leads to the fact that the expectant mother is often forced to rest. Some women increased daytime sleepiness. Night sleep is, on the contrary, violated. Often, expectant mothers suffering from changes in blood pressure complain of persistent insomnia and the appearance of restless frightening dreams.

How is the treatment carried out?
The choice of therapy will depend on a variety of baseline parameters. To normalize the level of blood pressure, doctors will definitely recommend that the expectant mother carefully monitor the daily routine. complete sleep, balanced diet and limitation of psycho-emotional stress are important factors in the treatment of any vascular disorders.
For women suffering from a persistent and pronounced increase in blood pressure, doctors will definitely recommend limiting significant physical activity. Especially under the ban on lifting weights.
In late pregnancy the expectant mother must carefully plan and observe her daily routine. Walking in the fresh air will have a positive effect not only on the mother's body, but will also be very useful for her baby.

If a woman has any dangerous pathology that could threaten her life or her baby, she will be hospitalized. AT medical institution she will receive all the necessary treatment.
In some situations, the expectant mother is in the hospital until the very birth. However, this option is possible with a really severe pathology that requires daily medical supervision.

It is very important to monitor blood pressure from the 36th week of pregnancy until the very birth. At this time, the female body is preparing for the upcoming birth of the baby. Any deviation from the norm of blood pressure requires a mandatory visit to the doctor for advice.
As you know, obstetric and calendar months do not match in duration. Therefore, the 35th week of pregnancy according to obstetric terms is the second half of the ninth month, and if you count according to calendar terms, it is the very beginning of the last month of gestation. Let's figure out what happens at week 35 and what difficulties may arise during this period.
So, you are at the 35th week of pregnancy, which means that there are still 4-5 weeks before the expected date of delivery. However, not all children are born on exactly the calculated dates. Many are “impatient” to be born, and childbirth can occur at any time. At the same time, the born baby will no longer be considered premature, although they will write to you in the certificate that “preterm birth” has occurred.
well-being
35 obstetric week of pregnancy is a continuation of the third trimester. This period is characterized by intensive growth of the fetus. And along with the fetus, the uterus also grows, which leads to the appearance of various unpleasant sensations. At 35 weeks pregnant, many women experience:
- Difficulty breathing, shortness of breath. This is due to the fact that the uterus literally supports the lungs. Do not worry, it will not be long to endure, the stomach should soon drop and breathing will immediately become easier.
- Digestive disorders. Most often, women complain of recurrent heartburn and constipation. These phenomena are due to the fact that the stomach and intestines are squeezed by a large uterus.
- Dizziness, weakness. The cause of discomfort is the compression of the inferior vena cava by the uterus. This leads to disruption of normal blood circulation. To avoid unpleasant phenomena, it is not recommended to stay in one position for a long time. It is especially dangerous to lie on your back for a long time.

- Edema. Swollen limbs in the evening is a problem that almost every pregnant woman faces. If the appearance of edema is not accompanied by an increase in blood pressure, then this is the norm at this time. Try to rest more lying down with a pillow under your feet.
- At this stage of pregnancy, weight, as a rule, reaches a maximum. Now the woman weighs significantly more than before pregnancy, and this makes it difficult to move and makes the woman clumsy. How many kilograms do women gain by the end of pregnancy? This indicator is individual, but the average increase is 9-12 kg.
- The uterus at thirty-five weeks is greatly stretched, so it often comes into tone. The tone of the uterus is manifested by the fact that the stomach becomes “stone”. Another reason that the stomach stiffens at 35 weeks of gestation and the uterus comes into tone is training contractions. In this case, as a rule, the lower abdomen slightly hurts, and the nature of the pain is pulling.
Training fights manifest themselves in different ways. Most often, the pain during them is insignificant, but in some women the lower abdomen at 35 weeks can hurt quite badly. But these pains are short-term, they last no more than 10 minutes. If at the 35th week of pregnancy the stomach hurts long time, and the pain becomes more intense, then you need to urgently call an ambulance.
- 35 obstetric week is the time when the fetus begins to gradually sink down. This can lead to discomfort between the legs (in the groin area). In addition, pulling pains in the lower abdomen at the 35th week of pregnancy may be due to the divergence of the pelvic bones and softening of the ligaments.

- The child at this stage cannot actively move, because the size does not allow him to roll over. Therefore, at the 35th week of pregnancy, fetal movements are expressed mainly by rather strong shocks.
Multiple pregnancy
The 35th week of pregnancy with twins is an extremely difficult period for a mother, because her body is experiencing a double load. It will be necessary to be ready that childbirth will begin at any moment. Indeed, due to strong stretching, the uterus comes into tone, and this can provoke the onset of labor.
If the children are in the correct position in the uterus, and the woman is generally healthy, then doctors may recommend natural childbirth. If one twin is located across the uterus, both children are in the breech presentation, or there are other indications, then the date of the planned caesarean section will be set. Perhaps the operation will take place exactly at 35 weeks.
Child development
Let's figure out what happens to the baby at 35 weeks of gestation. By this time, the development of the fetus is completed, it is completely ready for independent life, but the weight of the fetus at the 35th week of pregnancy is still insufficient. And, it is desirable that he still accumulate strength until the moment of birth.

On average, the weight of a child at 35 weeks of gestation is more than two kilograms. His skin every day becomes more and more light and smooth, the original fluff disappears, which previously covered the entire body. But the lubricant remains on the skin, because it protects the skin of the child from softening from constant exposure to the liquid.
In addition, the presence of lubrication is necessary in order to make it easier for the child to pass through the birth canal.
The fetus at 35 weeks of gestation has fairly dense bones and developed muscles. The only exceptions are the bones of the skull. On the head of the child there are soft areas - fontanelles, the largest of which will completely close only by the end of the first year of the baby's life. Meconium is already accumulating in the intestines - sterile original feces that will come out during the first hours of life.
Surveys
Most likely, the baby at 35 weeks is already in a position in which it will remain until childbirth. In most cases, the baby is head down. If it turns out that the child is in a different position, then the likelihood that he will roll over at this time is very small.
To control the position of the child, an ultrasound scan may be prescribed at 35 weeks of gestation. In the event that the child is head up, doctors will choose the tactics of childbirth. In some cases, a caesarean section is indicated.

Conducting ultrasound screening, the specialist will definitely pay attention to the position of the umbilical cord. Tight entanglement of the umbilical cord can cause hypoxia. In addition, during ultrasound, the condition of the placenta, which provides the connection between the mother's body and the fetus, is assessed. At this time, the normal indicator of the degree of maturity is the second.
Pregnancy 35 weeks is the period at which the following examinations can be scheduled:
- urinalysis is performed to monitor kidney function;
- A gynecological smear is taken to identify the composition of the microflora. If pathogenic flora (for example, fungi) is detected, it is necessary to undergo treatment before childbirth so as not to infect the child;
- a blood test for hemoglobin, glucose, as well as for infections - HIV, syphilis, hepatitis.
If indicated, other examinations may be prescribed.
Possible Complications
Pregnancy at 35 weeks may be overshadowed by the development of the following complications:
- Preeclampsia. This is an extremely dangerous condition for both mother and baby. It is manifested by an increase in blood pressure and impaired renal function. Monitoring of kidney activity is carried out through a weekly urine test. Edema at 35 weeks is also a sign of the development of preeclampsia.

- Placenta previa. If the placenta is located so that it partially or completely blocks the birth canal, then bleeding, premature birth, or fetal hypoxia may develop. The main sign of problems with the placenta is spotting at 35 weeks of gestation. But, as a rule, this complication is detected earlier, during a planned ultrasound.
- Placental abruption. Detachment of the placenta from the uterine wall can be partial or complete. In the first case, it is still possible to preserve the pregnancy, in the second, emergency medical care is required. The signs of complications are brown discharge or bleeding, as well as sharp pains.
Harbingers of childbirth
At the described period, the first harbingers of an early birth may already appear. Their appearance does not mean that you need to immediately go to the hospital. Often the appearance of the first precursors occurs a few weeks before childbirth.
However, remember that every pregnancy is different. Therefore, never rely on someone else's experience, and even on your own in a previous pregnancy. Sometimes harbingers appear almost before the very birth - in 1-2 days.

What are the signs to look out for? Many expectant mothers note that at this stage of pregnancy, the lower back is pulled. This is due to the load on the spine due to the displacement of the center of gravity of the figure. As a rule, the pain intensifies if the woman is in one position for a long time.
In addition, some women note that at the 35th week of pregnancy, the stomach dropped. You can notice this not only visually, but also physically. The uterus stops putting pressure on the diaphragm, so it becomes easier for a woman to breathe.
If at 35 weeks your pregnant belly hasn't dropped, don't worry. This significant event will take place in 1-2 weeks.
preterm birth
At this time, the likelihood of preterm birth is high. Do not be afraid, your baby is quite ready for independent life, so there is no threat to him. It’s just that he will be born with a lower weight, but will soon catch up with his peers who were born at a later date.

The main signs of precursors of preterm birth:
- Pulling the stomach at 35 weeks pregnant. That is, there are pains that are similar to pain during menstruation. Sometimes, in addition to pulling the lower abdomen, there are back pains that radiate to the sacrum;
- Tone of the uterus. This state is felt as tension, the stomach becomes hard.
- Chair disorder. Many women have diarrhea before childbirth.
- Sensation of pressure on the perineum.
- At the 35th week of pregnancy, discharge in the form of blood or abundant clear discharge (amniotic fluid may leak).
The main symptoms that childbirth has already begun:
- Removal of the mucous plug that covers the cervix. This plug looks like a collection of transparent or whitish mucus the size of Walnut with bloody patches in the form of veins;
- Discharge of water. This symptom is difficult not to notice, since about 0.5 liters of amniotic fluid is poured out at the same time.

- The appearance of contractions. True contractions are more intense than training contractions. They are more painful and happen at regular intervals. Moreover, these intervals are getting shorter, and the intensity of pain increases.
So, the 35th week of pregnancy is the perfect time to prepare all the things that you will need to take with you to the hospital. Of course, there is a chance that the pregnancy will last another 4, 5 or even 6 weeks, but it is better to be prepared for any surprises. In no case, do not go traveling during this period and, in general, try not to leave far from home. And if it is absolutely necessary, then keep documents and an exchange card with you.