Bones take on an irregular shape and position if professional help has not been provided after the fracture. The essence of this procedure is that the diseased bone is broken and then fixed with the help of special plates or other devices so that it grows together and takes its natural shape. Osteotomy is used to achieve the following goals:
- return motor functions to the limbs, restore their performance;
- in the practice of plastic surgery, osteotomy is used to lengthen the limbs;
- restore the base function.
Depending on the purpose of the procedure, the object of osteotomy changes. Say, in order to return the support function, this procedure is performed on the hip joint.
Corrective osteotomy is aimed precisely at restoring the position, shape and performance of the limbs after an illness or injury.
The process of the procedure
Training
The process of preparation for this operation consists in an extensive radiograph, during which the orthopedic surgeon receives images of the area that can be corrected from different angles. Thus, he chooses the optimal tactics for conducting the operation.
Corrective osteotomy procedure
Those bone structures that are subject to adjustment are artificially broken by an orthopedic surgeon during the operation, and then fixed at the right angle and in the required position. In order for the bones to grow together correctly, a special plate or other special means, such as knitting needles and bolts, are installed. Thanks to modern technologies and in order to avoid complications in the form of contractures in adjacent joints, gypsum is not applied.
rehabilitation period
Rehabilitation lasts depending on which part of the body was operated on, for example, corrective osteotomy of the knee joint requires 12 weeks of rehabilitation. Moreover, the bones grow together for the first two months, the rest of the time they acquire the necessary strength. During this period of time, loads on the operated part of the body are excluded.
Indications
Corrective osteotomy is indicated for malunion of fractures. In addition, diseases such as:
- different types of arthrosis, including osteoarthritis and gonarthrosis;
- ankylosis of bones;
- rickets.
In addition, this operation is performed to delay the need to replace the joint with an artificial one, as well as to correct the prosthesis.
Contraindications
Osteotomy is contraindicated in diseases of the kidneys and liver, in disorders of the cardiovascular system. It can not be carried out if the patient has an exacerbation of any chronic disease, as well as in acute diseases. It is impossible to do an osteotomy for those who suffer from any diseases of a purulent nature.
Complications
This surgical operation is complex and quite risky. The following complications may occur:
- slow fusion of bones;
- the formation of suppuration;
- incorrect change in the position of the wreckage;
- the appearance of a false joint.
Prices and clinics
This operation is carried out only in well-equipped medical centers. For its implementation, specific experience of the doctor is required. Prices for corrective osteotomy depend on the nature and complexity of the operation.
1The article is devoted to the topical issue of modern orthopedics - corrective osteotomies in the knee joint. The aim of the work is to review the current literature to summarize the data of domestic and foreign researchers, determine the indications for performing corrective osteotomies, the level and degree of correction of the axis of the lower limb. The results of studies of the influence of the position of the mechanical axis of the lower limb on the distribution of contact pressure in the joint are shown. Methods for determining the necessary degree of correction to achieve a normal mechanical axis of the lower limb are considered. Literature data on the results of normalization of axial deformities in the treatment of deforming arthrosis of the knee joint were analyzed. The use of this technique is advisable in young patients with gonarthrosis of the second or third stage. To obtain good long-term results, it is necessary to correctly and accurately follow the indications for performing corrective osteotomy, and to perform the most accurate calculation of the correction.
lower limb axis
gonarthrosis
corrective osteotomy
1. Bagirova, G.G. Osteoarthritis: epidemiology, clinic, diagnosis, treatment / G.G. Bagirova, O.Yu. Meiko. - M., 2005.- 224p.
2. Bragina, S. V. The structure of persistent disability in patients with gonarthrosis / S. V. Bragina, R. P. Matveev / / Orthopedic Genius. - 2011. - No. 4. - P.101-105.
3. Golovakha, M.L. Long-term results of high corrective osteotomy of the tibia in gonarthrosis / M.L. Golovakha, V. Orlyansky / / Orthopedics, traumatology and prosthetics. -2013. - No. 1. - P.10-15.
4. Zaitseva, E.M. Causes of pain in osteoarthritis and factors of disease progression (literature review) / E.M. Zaitseva, L.I. Alekseeva // Scientific and practical rheumatology. - 2011. - No. 1. - P. 50–57.
5. Zorya, V. I. Deforming arthrosis of the knee joint: a guide for doctors / V. I. Zorya, G. D. Lazishvili, D. E. Shpakovsky. - M.: Litterra, 2010. - 320 p.
6. Kolesnikov, M.A. Modern methods of treatment of gonarthrosis (literature review) / M.A. Kolesnikov, I.F. Akhtyamov // Bulletin of traumatology and orthopedics of the Urals. - 2012. - No. 1-2. - P. 121-129.
7. Kornilov, N.N. Modern ideas about the advisability of using corrective periarticular osteotomy in deforming arthrosis of the knee joint / N.N. Kornilov, K.A. Novoselov, T.A. Kulyaba // Bulletin of Traumatology and Orthopedics. N.N. Priorov. - 2004. -№3.-S. 91-95.
8. Kotelnikov, G.P. Surgical correction of deformities of the knee joint / G.P. Kotelnikov, A.P. Chernov. - Samara, 1999.- 180 p.
9. Loskutov, A.E. Arthroscopy and corrective osteotomy in the treatment of gonarthrosis / A.E. Loskutov, M.L. Golovakha // Visn. orthopedist, traumatologist that prosthesis. - 2002. - No. 2. − P. 5–7.
10. Makushin, V.D. Gonarthrosis: long-term results of the use of high valgus osteotomy of the tibia (review of foreign literature) / V.D. Makushin, O.K. Chegurov // Genius of Orthopedics. - 2007.- No. 1.- P.137-143.
11. Matveev, R.P. Osteoarthritis of the knee joint: problems and social significance / R. P. Matveev, S. V. Bragina / / Human Ecology. - 2012. - No. 9. - P. 53-62.
12. Mironov, S.P. Osteoarthritis: current state of the problem / S.P. Mironov, N.P. Omelyanenko, A.K. Orletsky // Bulletin of Traumatology and Orthopedics. N.N. Priorov. - 2001. - No. 2. - S. 96-99.
13. Muller, B. High tibial osteotomy: conditions, indications, technique, problems, results / V. Muller // MargoAnterior. - 2003. - No. 1−2. – S. 2−10.
14. Orlyansky, V. Corrective osteotomy in the area of the knee joint / V. Orlyansky, M.JI. Holovakha, R. Shabus - Dnepropetrovsk: Thresholds, 2009.- 159 p.
15. Planning the amount of correction for corrective osteotomy of the tibia / M.L. Golovakha, I.V. Shishka, O.V. Banit, V. Orlyansky// Orthopedics, traumatology and prosthetics.−2010.−№1.−S. 91–97.
16. A ten-to 15-year follow-up observation of high tibial osteotomy in medial compartment osteoarthrosis/ Yasuda K. //Clin.Orthop.Relat.−1992.−vol.282.−P.186-195.
17. Aglietti, P. Tibial osteotomy for the varus osteoarthritic knee/ P. Aglietti, E. Rinonapoli// Clin. Orthop.- 1983.-№176.-P. 239-251.
18. Agneskirchner, J.D.. The effects of valgus medial opening wedge high tibial osteotomy on articular cartilage pressure of the knee: a biomechanical study/ J.D. Agneskirchner // Arthroscopy.- 2007.-vol.23, No. 8.-R.852-861.
19. Amendola, A. High tibial osteotomy for the treatment of unicompartmental arthritis of the knee/ A. Amendola, L. Panarella // Orthop. Clin. North. Am. - 2005. - vol. 36, No. 4. - R. 497-504.
20. Arden, N. Osteoarthritis: epidemiology / N. Arden, M.C. Nevitt // Best Pract. Res. Clin. Rheumatol. - 2006.-vol.20, No. 1.-P. 3-25.
21. Association between valgus and varus alignment and the development and progression of radiographic osteoarthritis of the knee/ G.M. Brouwer, A.W. van Tol, A.P. Bergink, J.N. Belo, R.M. Bernsen, M.Reijman //Arthritis Rheum.- 2007.-vol.56, No. 4.-P.1204-1211.
22 Bae, D.K. Total knee arthroplasty following closed wedge high tibial osteotomy / D. K. Bae, S. J. Song, K. H. Yoon // International Orthopedics (SICOT).- 2010. -vol.34.-P.283-287.
23. Brinkman, J.M. Osteotomies around the knee: patient selection, stability of fixation and bone healing in high tibial osteotomies/ J.M. Brinkman // J. Bone Jt. Surg. - 2008. - Vol. 90, No. 12. - R. 1548-1557.
24. Cole, B. Degenerative arthritis of the knee in active patients: evaluation and management / B. Cole, C. Harner // J. Am. Acad. Orthop. Surg. - 1999. - Vol. 7, No. 6. - P. 389-402.
25. Coventry, M. Proximal tibial osteotomy. A critical long-term study of eighty-seven cases / M. Coventry, D. Ilstrup, S. Wallrichs // J. Bone Jt. Surg. - 1993. - vol.75-A, No. 2. - P. 196-201.
26. Doherty, M. Risk factors for progression of knee osteoarthritis / M. Doherty // Lancet. - 2001. - Vol. 358. - P. 775.
27. Esenkaya, K. Proximal tibial osteotomies for the medial compartment arthrosis of the knee: a historical journey / K. Esenkaya, U. K. Akan // Strat. Traum. Limb Recon.−2012.−№7.−Р.13–21.
28. Frey, P. Closing-wedge high tibial osteotomy with a modified Weber technique/ P. Frey, M. Muller, U. Munzinger // Oper. Orthop. Traumatol.-2008.- vol.20, no.1.- P.75-88.
29. Frontal Plane Knee Alignment: A Call for Standardized Measurement / T. D. Cooke, E. A. Sled, R. A. Scudamore // J. Rheum.-2007.- vol. 34, No. 9. − P. 1796 - 1801.
30. Fujisawa, Y. The effect of high tibial osteotomy. An arthroscopic study of 26 knee joints / Y. Fujisawa, K. Masuhara, N. Matsumoto I IClin. Orthop. Surg. - 1976. - Vol. 11. - P. 576-590.
31. Giagounidis, E. M. High tibial osteotomy: factors influencing the duration of satisfactory function / E. M. Giagounidis, S. Sell // Arch. Orthop. Trauma Surg. - 1999. - vol.119, No. 7-8. - P. 445-449.
32. Hernigou, P. A 20-year follow-up study of internal gonarthrosis after tibial valgus osteotomy. Single versus repeated osteotomy / P. Hernigou // Rev. Chir. Orthop. - 1996. - Vol. 82, no. 3. - P. 241-250.
33. Hofmann, S. Principles and indications of osteotomies around the Knee/S. Hofmann, M. Pietsch// Arthroskopie.−2007.− vol.20, No. 4.−Р. 270-276.
34. Insall, J.N. High tibial osteotomy for varusgonarthrosis: a long term follow-up study/ J.N. Insall, D.M. Joseph, C. Lsika // J Bone Jt. Surg.- 1984.-vol.66-A, No. 7.-R.1040-1048.
35. Jackson, J. Tibial osteotomy for osteoarthritis of the knee /J. Jackson, W. Waugh // J Bone Joint Surg.-1961.- vol.43-B, no. 4.-P.746-751.
36. Jacob, R. Tibial osteotomy for varusgonarthrosis: indication, planning and operative technique / R. Jacob, S. Murphy // AAOS Instr. Course Lect. - 1992.-Vol. 41.-P. 87-93.
37. Karabatsos, B. Functional outcome of total knee arthroplasty after high tibial osteotomy/ B. Karabatsos, N.N. Mahomed, G.L. Maistrelli // Can. J. Surg. - 2002. - vol. 45, No. 2. - R. 116-119.
38. Koshino, T. Medial opening-wedge high tibial osteotomy with use of porous hydroxyapatite to treat medial compartment osteoarthritis of the knee/ T. Koshino, T. Murase, T. Saito// J. Bone Jt. Surg.- 2003.-vol.85-A, No.1.-R.78-85.
39. Kolb, W. Opening-wedge high tibial osteotomy with a locked low-profile plate / W. Kolb, H. Guhlmann, C. Windisch // J. Bone Jt. Surg.-2009.- Vol.91-A, No. 11.-R.2581-2588.
40. Lobenhoffer, P. Open valgus alignment osteotomy of the proximal tibia with fixation by medial plate fixator/ P. Lobenhoffer, J. Agneskirchner, W. Zoch //Orthopade.- 2004.- vol.33, No. 2.- P. 153-160
41. Maquet, P. Arthritis of the knee / P. Maquet. - New York: Springer-Verlag, 1980. - 183 p.
42. Moreland, J. R. Radiographic Analysis of the Axial Alignment of the Lower Extremity / J. R. Moreland, L. W. Basset, G. J. Hanker // J. Bone Jt. Surg.-1987.- vol. 69-A, No. 5.-P. 745-749.
43. Noyes, F.R. Opening wedge tibial osteotomy: the 3-triangle method to correct axial alignment and tibial slope/ F.R. Noyes, S.X. Goebel, J. West //Am. J. Sports Med. - 2005. - vol. 33, No. 3. - R. 378-387.
44. Paley, D. Principles of deformity correction/ D.Paley. − New York: Springer-Verlag, 2003. − 806 p.
45. Parvizi, J. Total knee arthroplasty following proximal tibial osteotomy: risk factors for failure / J. Parvizi, A.D. Hansen, M.J. Spangehl // J. Bone Jt. Surg.- 2004.-vol.86.- P.474-479.
46. Prospective outcomes of young and middle-aged adults with medial compartment osteoarthritis treated with a proximal tibial opening wedge osteotomy /R. F. LaPrade // Arthroscopy: The Journal of Arthroscopic and Related Surgery.−2012.−vol.28, №3.−P. 354-364.
47. Relationship between pain and medial knee joint loading in mild radiographic knee osteoarthritis/L.E. Thorp et al.//Arthritis Rheum.- 2007.- vol.57.- P. 1254-1260.
48. Rinonapoli, E. Tibial osteotomy for varusgonarthrosis: a 10- to 21-year follow-up study / E. Rinonapoli, G. Mancini, A. Corvaglia / Clin. Orthop. - 1998.-Vol. 353.-p. 185-193.
49. Sharma, L. The Role of Varus and Valgus Alignment in Knee Osteoarthritis/ L. Sharma // Arthritis Rheum.−2007.− vol. 56, No. 4.−Р.1044–1047.
50. Spahn, G. Complications in high tibial (medial opening wedge) osteotomy/ G. Spahn // Arch. Orthop. Trauma Surg.-2003.-vol.124.-P. 649–653.
51. Sprenger, T.R. Tibial Osteotomy for the Treatment of Varus Gonarthrosis: Survival and failure analysis to twenty-two years/ T. R. Sprenger, J. F. Doerzbacher /// J. Bone Jt. Surg.-2003.-vol.85-A, No.3.-P.469-474.
52. Ten-year results of tibial osteotomy for medial gonarthrosis. The influence of overcorrection / S. Odenbring // Arch. Orthop. Trauma Surg. – 1991.–vol. 110, no. 2. - P. 103-108.
53. W-Dahl, A. High tibial osteotomy in Sweden, 1998–2007. A population-based study of the use and rate of revision to knee arthroplasty/ A.W-Dahl, O. Robertsson, L. S. Lohmander// ActaOrthopaedica.− 2012.− vol. 83, No. 3.-P. 244–248.
54. Wildner, M. Complications of high tibial osteotomy and internal fixation with staples/ M. Wildner, A. Hellich, A. Reichelt // Arch. Orthop. Trauma Surg.–1999.–vol.111, No. 4. - P. 202-210.
55. Zaki, S.H. High tibial valgus osteotomy using the Tomofix plate –medium-term results in young patients/S.H.Zaki, P.J. Rae // ActaOrthop. Belg.-2009.- vol.75, no.3.-R.360-367.
Deforming diseases of the joints of degenerative-dystrophic origin are widespread among the adult population and account for more than 8-12%. In the structure of degenerative-dystrophic diseases of the joints, the knee joint accounts for 33.3% of cases. In recent years, there has been a tendency to increase the incidence of deforming arthrosis among people of young working age, which significantly increases the social significance of the problem. There is an increase in the incidence of arthrosis among people of the middle age group (40-60 years) up to 60%, and the duration of the period of disability increases. Conservative treatment does not always bring a positive effect, which leads to a decrease in the quality of life of patients. In young patients, the question of the need for surgical intervention is inevitably raised in order to prevent the progression of arthrosis and the transfer of knee arthroplasty to a later date.
Recently, operations to correct the axis of the lower limb for the treatment of gonarthrosis are again increasingly used, especially in young patients. It is known that corrective osteotomies have been used since the 19th century, when A. Meyer first used this technique for the treatment of gonarthrosis. In the 20th century, J.P.Jackson, W.Waugh, M.Coventry, T.Koshino, P.Maquet made a great contribution to the popularization of corrective osteotomies. Currently, R. Lobenhoffer is actively promoting the use of these operations.
Since the second half of the 20th century, in the treatment of gonarthrosis, knee arthroplasty has become the method of choice among surgical interventions. Corrective osteotomies, as a method of surgical intervention, have faded into the background, if not completely forgotten. In this article, we will try to consider the views of orthopedists on the use of osteotomies in the treatment of degenerative-dystrophic diseases of the knee joint.
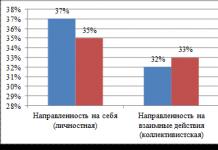
Today, deforming arthrosis is recognized as a polyetiological disease. Many scientists studying the pathogenesis of osteoarthritis are supporters of the mechano-functional theory of the development of deforming arthrosis of the knee joint. According to this theory, the development of a degenerative-dystrophic process in the articular cartilage, subchondral bone, and joint capsule is associated with a functional overload of the cartilage due to a large amount of load. Axial deformities lead to premature disproportionate wear of the knee joint with the development of degenerative-dystrophic changes. Some scientists have expressed the opinion that the disease is based on a discrepancy between the functional load on the cartilage and its biological capabilities.
The influence of the position of the mechanical axis of the lower limb on the distribution of contact pressure in the joint has been the subject of a number of experimental studies. The most modern method for studying contact pressure is the use of a measuring foil, which operates on the basis of the Tekscan-System electromechanical resistance principles (Fig. 1.). Riegger-Krugh investigated the distribution of loads in the knee joint after osteotomies on cadaveric material. Modeled varus deformity, and then performed osteotomy. The authors found an expected increase in loads in the medial region with varus deformity and in the lateral region with valgus deformity. The work is interesting in that with the neutral axis of the knee joint, the load fell more on the lateral part of the joint. After correction, the same load data are obtained as with the normal axis.

Rice. 1. Examination of pressure distribution in the knee joint using the Tekscan-System.
The idea of corrective osteotomy is that due to the normalization of the axis of the lower limb, the load is redistributed from the damaged section of the joint subjected to significant loads to a relatively healthy one. Osteotomies in the area of the knee joint are divided according to the level of correction: at the level of the femur; at the level of the lower leg - high and low tibial, and are also divided according to the method of crossing the bone and the nature of the correction: transverse, spherical, straight, oblique, opening, closing. Currently, the most commonly used high opening wedge osteotomy, which allows you to solve almost all the technical difficulties that arise when normalizing the axis of the lower limb. It should also be noted the importance of using adequate, stable fixators when fixing bones after osteotomy. Previously, after the normalization of the limb axis by surgery, patients were forced to use various methods of immobilization for a long time, which significantly lengthened the rehabilitation period. In the 2000s, at the height of the new development of osteotomies, many manufacturing companies offered their fixation options, which can significantly reduce the recovery time after this operation. The use of modern fixators makes it possible to start a partial load on the limb in the first days after the operation and, of course, to exclude long-term immobilization, and in some cases to refuse it.
Corrective osteotomies are considered as a complementary method, preparing for arthroplasty, and in some cases, axis correction operations can do without prosthetics. In order for corrective osteotomies in the area of the knee joint to bring a lasting effect, it is necessary: to correctly determine the indications; adequate preoperative examination; calculate the degree and level of correction.
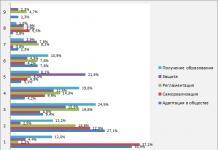
A good result in the correction of the axis of the lower limb can only be obtained with the right choice of indications. If corrective osteotomy is performed without taking into account the necessary factors, at best it can do no harm, and at worst, accelerate the destruction of the joint. The experience of modern orthopedists was summarized in 2009 at a meeting of the International Society of Arthroscopy, Knee Surgery and Orthopedic Sports Medicine and is reflected in Table 1.
Table 1
Indications, relative indications and absolute contraindications for corrective osteotomies
|
Indications |
Relative readings |
Absolute contraindications |
|
Age up to 60 years |
Age after 60 years |
Rheumatoid arthritis |
|
Deforming arthrosis 2 tbsp. |
Deforming arthrosis 3 tbsp. |
|
|
Absence of patellofemoral arthrosis |
Moderate patellofemoral arthrosis |
Patello-femoral arthrosis 3 tbsp. |
|
Varus, valgus< 15 гр. |
Instability of PKS, ZKS. |
Arthrosis of the contralateral joint. |
|
Isolated arthrosis 2-3 tbsp. |
Isolated arthrosis 3-4 tbsp. |
Osteoporosis |
|
Range of motion>100 gr. |
Range of motion >90 gr. |
Flexion limit >25 gr. |
|
Full extension |
Contralateral meniscectomy |
|
|
High degree of initial activity |
Meniscectomy |
Decreased blood flow through the vessels of the n / limb |
|
Normal contralateral joint component |
Dissecting osteochondritis |
Extra-articular deformities |
|
Stable knee joint, intact cruciate ligaments |
Necrosis of the condyles of the femur |
Decreased bone regeneration |
|
Intact menisci of the knee joint |
Flexion limit > 15 gr. |
Previous infection |
|
Varus, valgus deformity more than 15 gr. |
As a preparation for surgical treatment, it is necessary to conduct a thorough examination before the intervention, which includes clinical and laboratory tests, and, according to most orthopedists, it is imperative to perform images of the lower limb throughout - a teleroentgenogram (FLFS) (Fig. 2).
Rice. 2. Pictures of the lower limb throughout.
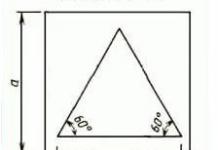
To correctly determine the level of osteotomy and the degree of necessary correction on images of the lower limb throughout, it is necessary to distinguish between the relationship of the following axial ratios and angles in the area of the knee joint (Fig. 2):
Anatomical-mechanical angle (AMU) = 6±1° - the angle between the anatomical and mechanical axes of the femur (1).
Mechanical distal femorolateral angle (MDFLU) = 87±3° (2).
Mechanical proximal mediotibial angle (MPMT) = 87±3°(3).
The anatomical axis of the lower limb (4) corresponds to the longitudinal axes of the femur and tibia.
The mechanical axis of the lower limb (Mikulich line) (5) passes through the center of the femoral head, through the center of the knee joint and through the center of the ankle joint.
Anatomical femorotibial angle (AFTU) = 173-175° - this angle is formed by the anatomical axes of the femur and tibia (6).
The line of the knee joint in the frontal plane has a bevel relative to the midline of about 2 degrees from the outside inwards (7).
Tibial slop 5-10° - posterior slope of the tibial plateau.
The main indications for performing corrective osteotomies in the area of the knee joint are: displacement of the mechanical axis of the lower limb medially or laterally by 10 mm from the midline, as well as a change in MDFLU and MMPTU by more than 3 degrees.
There are many methods for determining the degree of correction required to achieve a normal mechanical axis of the lower limb. One of the very first calculation methods was proposed by Coventry, which consists in calculations along the anatomical axis or along the biomechanical axis. Of the more modern techniques, it is necessary to note preoperative planning according to Lobenhoffer, in which it is necessary to focus on the passage of the mechanical axis through the Fujisawa point. The most commonly used preoperative planning is Miniation. Its essence is as follows: a radiograph of the entire lower limb is needed, planning also takes place taking into account the Fujisawa point. The Fujisawa point is an anatomical landmark located on the mechanical axis of the lower limb on the plane of the tibia through a point in the lateral compartment at a distance of 62% of the total width (provided that the countdown starts: from 0% of the medial edge to 100% at the lateral edge), which is the best location for the corrected mechanical axis (Fig. 3). This is consistent with the results reported by Noyes. The scientists obtained the same results, indicating that the shift of the load to the medial third of the lateral compartment reduces the degenerative change of the articular cartilage, while some restructuring of the cartilage layers is observed.

Fig.3. Anatomical landmark - point Fujisawa.
When planning for Miniation, the following auxiliary lines must be used:
Line 1 runs from the femoral head (from its center) through the Fujisawa point of the total width of the tibial plateau lateral to the center of the knee joint to the plane of the ankle joint. This line represents the desired postoperative limb axis.
Line 2 starts from the center of the proposed osteotomy - point "D", which is the final planned osteotomy. This line goes down and connects the point "D" with the center of the ankle joint on the radiograph.
Line 3 connects point "D" with a point on line 1, which is located at its intersection with the plane of the ankle joint.
The open angle between lines 2 and 3 (Angle Alpha) is the desired angle for the required correction (Fig. 4).

Rice. 4. Planning the amount of correction according to Miniazi.
Only by using the correct indications and carefully calculating the degree of correction can positive and long-term results be expected. When analyzing literature sources, the following data on the effectiveness of osteotomies were obtained (Table 2).
table 2
Long-term results of corrective osteotomies
|
Quantity |
Result |
|
|
86% saving effect 5 years 74% saving effect 10 years 56% saving effect 15 years |
||
|
85%good 5 years 63% good 9 years old |
||
|
88% good 7 years old 78% good 10 years 57% good 15 years old |
||
|
Billings |
85% good 5 years 63% good 10 years |
|
|
87% good 5 years 69% good 10 years |
||
|
94% good 5 years 85% good 10 years 68% good 15 years old |
||
|
80% good 10 years 10% good 15 years |
||
|
80% good 5 years 58% good 10 years |
||
|
88% good 6 years old 63% good 10 years |
||
|
Matthews |
50% good, satisfactory 5 years 28% good 9 years |
|
|
51% good 9 years |
||
|
55% good 15 years |
||
|
81% good 11 years old |
||
|
91% good 5 years |
||
|
73% good 9 years old |
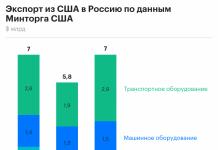
The data of the Swedish registry for 1998-2007 shows a generalized result of performing corrective osteotomies (3161 operations) and subsequent total knee arthroplasty (Fig. 5).

Fig.5. Endoprosthetics after corrective osteotomy (Swedish registry data).
The researchers note that during this period of observation, radiographically revealed no signs of progression of arthrosis, and only sometimes they note some deterioration in the contralateral section of the joint.
The results of studies on the use of total knee arthroplasty after corrective osteotomy were analyzed. There are publications on the difficulties of using arthroplasty after corrective osteotomy, in which an increase in the number of complications up to 30% is noted. Nevertheless, most orthopedists are inclined to believe that when performing correctly calculated osteotomies, primary arthroplasty does not differ in any technical features. Moreover, the implantation of the endoprosthesis in the conditions of normal anatomy of the knee joint brings the best long-term results.
And the last of the issues regarding osteotomies, which is widely covered in the literature, is complications. Complications of corrective osteotomies include progression of the process, lack of consolidation, infection, loss of correction, neuropathy of the tibial nerve.
Thus, in conclusion, we can say that corrective osteotomies, as a method of treating gonarthrosis, are still relevant. It is advisable to use this technique in young patients with gonarthrosis of the second or third stage. In addition, it is necessary to correctly and accurately observe the indications, calculate the correction, which allows you to get good long-term results.
Reviewers:
Yezhov I.Yu., Doctor of Medical Sciences, Head of the Trauma and Orthopedic Department, Associate Professor of the Department of Surgery, Nizhny State Medical Academy, FBUZ "Privolzhsky District Medical Center" of the Federal Medical and Biological Agency, Nizhny Novgorod.
Korolev S.B., Doctor of Medical Sciences, Professor, Head of the Department, State Budgetary Educational Institution of Higher Professional Education "NizhGMA" of the Ministry of Health of Russia, Nizhny Novgorod.
Bibliographic link
Zykin A.A., Tenilin N.A., Malyshev E.E., Gerasimov S.A. CORRECTIVE OSTEOTOMY IN THE TREATMENT OF GONATHROIS // Modern problems of science and education. - 2014. - No. 4.;URL: http://science-education.ru/ru/article/view?id=14032 (date of access: 01.02.2020). We bring to your attention the journals published by the publishing house "Academy of Natural History"
Osteotomy is an operation that is performed to cut the bone, which helps to cure certain diseases, both congenital and acquired. Speaking more generally, it is aimed at breaking the bone, after which measures are taken for its further, correct, fusion.
Main types
This method of surgical intervention is used under general anesthesia, and only on the bones of the lower or upper extremities. Today it is customary to distinguish between such types of osteotomy as:
- Transverse.
- Z - figurative (scarf-osteotomy)
- oblique
- Staircase.
- Angular
- Arcuate.
- wedge-shaped.
The operation can be performed by closed or open method. In the first case, a small incision is made on the skin - no more than 2 cm long, after which the bone is blindly crossed with a chisel. Moreover, you need to work with a chisel very carefully, and at the very end, when the bones are connected to each other by a small bridge, just break them. This is done to avoid damage to vessels and nerves that may be located deeper than the level of the proposed fracture.
This type is used extremely rarely and in most cases an open osteotomy is used, where everything is done under the strict visual control of the surgeon.
Operation goals
Corrective osteotomy of the knee joint is a very effective operation that helps patients get rid of such a serious pathology as deforming arthrosis. At the same time, it is quite realistic to delay the installation of an artificial joint for a long time, which can be from 5 to 10 years, and sometimes longer.
The meaning of the procedure lies in the artificial fracture of the lower leg and its subsequent connection with plates. As a result, defects that previously prevented patients from leading an active lifestyle are corrected, and after the complete healing of such a fracture, they can again play football, ski, and engage in active sports. At the same time, pain and deformity of the joint disappear for a long time.
Corrective osteotomy can be used for almost any bone of the extremities, whether it be the lower leg, thigh, foot bones, and even fingers.

Contraindications and indications
There are some diseases when such surgical intervention is strictly contraindicated. These include:
- Patello-femoral arthrosis of the 3rd degree.
- Arthrosis of the contralateral joint.
- Obesity.
- extra-articular deformities.
- Decreased bone regeneration.
- The presence of an infectious process.
As for the indications, everything here is strictly individual and everything depends not only on the existing diseases, but also on the patient's age, body weight, and the presence of other pathologies.
For example, an osteotomy of the knee joint can be performed provided that the person is not yet 60 years old. If this age is exceeded, then the issue is resolved strictly individually. Also, the main indications for this surgical intervention include:
- 2 degrees.
- Absence of patellofemoral arthrosis.
- The presence of valgus or varus no more than 15 degrees of curvature.
- Isolated arthrosis of 2-3 degrees.
- Full knee extension.
- Intact cruciate ligaments.
- Intact menisci of the knee joint.
Preparation and rehabilitation
Corrective osteotomy of the tibia or knee requires careful preparation from both the patient and the clinician.
The patient must undergo a complete examination, which includes blood and urine tests, a biochemical blood test, a blood sugar test, an X-ray examination of not only a possible site of an artificial fracture, but of the entire limb, a fluorographic examination of the lungs, a study for infections such as AIDS, syphilis, hepatitis.
As a rule, the operation is carried out according to plan, the patient can take all the necessary tests at the nearest clinic. On the appointed day, the patient is admitted to the hospital. The length of stay in the clinic after surgery is no more than 5 days. Outpatient rehabilitation can last 4 weeks or more. As for disability, this is decided strictly individually and usually this period is from 2 to 6 weeks. But here it all depends on the place of the osteotomy - foot, knee or thigh.
As for rehabilitation, electromuscular stimulators, magnetotherapy and lymphatic drainage can be used here. It is obligatory to wear an orthosis, which ensures the immobility of the operated bone.
Corrective osteotomy of the foot is a type of surgical intervention performed on deformed limbs. The essence of the operation is an artificial fracture of the bones to correct the defect.
Every third inhabitant of the planet suffers from articular syndrome. Rheumatoid arthritis, rheumatism, systemic lupus erythematosus, fractures, birth defects cause pathological changes in the joints. The problem is solved conservatively or surgically. Therapeutic tactics depend on the severity of the pathology, the duration of the process, the data of laboratory, instrumental research methods.
It is carried out on the tibia, ankle, knee, hip, shoulder joints. Quality operations stop the disease. The patient returns to normal life thanks to modern methods of treatment.
Osteotomy is an alternative to arthroplasty. It is carried out in adults and children.
The main indications for the technique:
- The child suffers from congenital anomalies of the skeleton.
- Incorrect union of the fracture, the formation of a false joint.
- Deforming changes in the feet occur as a result of a severe disease of the bone tissue.
- Ankylosis is manifested by a complete loss of joint movement. Surgical intervention helps restore the function of the damaged limb.
- It is carried out with a hammer-shaped deformity of the fingers.
- Severe forms of clubfoot. Poorly amenable to conservative treatment.
- Indicated for flat feet.
- With valgus deformity of the first finger, surgical intervention is resorted to.

Types and forms of the procedure
Osteotomy corrects deformity of the foot in various areas. The method of the procedure is determined by the severity of the condition, the pathological area, indications and contraindications for the technique.
There are the following types:
Z-shaped or scarf-osteotomy is performed in patients with hallux valgus. The deformity is manifested by an inward curvature of the limb. The disease affects mainly the distal parts of the legs. Pathology occurs in the area of the thumbs. Physiotherapy, massage and scarf osteotomy allow you to get rid of foot valgus: restore the normal structure and function of the feet.
The technique has a number of advantages:
- corrects complex changes in the anterior part of the foot;
- allows for lateral displacement of bone fragments;
- well tolerated by patients;
- rarely accompanied by complications;
- the rehabilitation period is short (1-1.5 months);
- a scarf osteotomy can make the metatarsus shorter/longer if needed;
- the technique allows to reduce the load on the first phalanx. The surgeons move the fragments down. Does not affect limb function.
With valgus of the feet, a bump appears on the thumb. Provides discomfort and pain. Scarf osteotomy allows you to remove the growth. The doctor fixes the fragments with the help of special screws.
A wedge osteotomy is performed on the first toe. The main indications are the short first metatarsal bone, hallux valgus. The main stages of surgical intervention include:
- the surgeon makes an incision from the medial side of the first finger to the lateral;
- further shifts the phalanx inward;
- rotates the finger to a physiological position.
Osteotomy of the metatarsal bone is a simultaneous operation. It is used in combination with other surgical techniques to correct foot defects.
Angular allows you to give the correct position due to the bilateral excision of tissues. During the procedure, the surgeon cuts tissue at an angle from both sides. Bones become in a physiological position.
The linear form of the disease is divided into oblique and transverse. The essence of the operation is to align with a transplant.
Chevron osteotomy of the 1st metatarsal bone of the foot is used to treat valgus deformity of the first toe. The angle between the first and second phalanx is corrected.
The chevron shape has positive aspects:
- after the procedure, a long-term therapeutic effect is maintained;
- simplicity and safety of implementation;
- allows you to restore the lost functions of the limb in full.
The course of the operation includes the following steps:
- The surgeon makes a Y-shaped incision in the joint capsule.
- It releases the head of the metatarsus from the tendons. Carries out a V-shaped cut to fully release the head.
- Then the doctor brings the metatarsal head out and fixes it with a screw. The rest of the bone is excised.
- Restores the integrity of the joint capsule and sutures the wound.
- The sutures are removed 5-7 days after the operation.
There are other ways to treat the foot (McBride, Sheda, Silver surgery, laser correction). The type of surgical intervention depends on the indications and localization of the pathology.
A qualified specialist will carry out the operation with high quality. There are two types of intervention:
- Closed - access is made through a small incision in the skin. The surgeon works blindly with a chisel. Requires high qualification, experience of the doctor. Wrong actions can result in damage to blood vessels and nerves.
- The open method allows you to fully visualize the damaged area through a large incision.

How is a corrective osteotomy performed?
Manipulation of the forefoot is carried out in a planned manner. Before the operation, a complete examination package is prescribed:
- A general analysis of blood and urine allows you to assess the state of the hematopoietic and renal systems. Intervention can be carried out in the absence of pathological changes in the analyzes.
- Blood sugar is tested to rule out diabetes. With high glucose levels, the procedure cannot be performed.
- A biochemical blood test allows you to evaluate the functions of the kidneys and liver, a coagulogram - blood clotting.
- Fluorography of the lungs, ECG are carried out without fail.
- To visualize the pathology, assess the degree of changes, the patient is sent for x-rays, computed tomography.
Corrective osteotomy on the forefoot is performed in several stages:
- The patient is given general/spinal anesthesia.
- The surgeon cuts the lateral surface of the foot.
- Performs bone spraying using one of the methods described above.
- Sets the joint of the first metatarsal bone in the correct position.
- Removes a bump.
- Fixes the first phalanx with screws or knitting needles.
- The surgeon restores the anatomical position of the ligaments and tendons.
- Next, sutures are applied to the skin.
After the operation, the patient is in the hospital for 3 days. Doctors monitor the patient's condition: temperature, blood pressure, pulse, respiratory rate, pulse oximetry. It is forbidden to load a sore leg. Wear hard-soled shoes for several months. Elastic bandaging of limbs is prescribed to prevent complications.
Make a control x-ray. It allows you to determine the degree of fusion, the overall dynamics. If there are no complications, doctors are allowed to give the leg a load. Over time, the patient can walk long distances, run, play sports.
Contraindications for surgery
Drug treatment of various deformities of the lower extremities is carried out for several months, years. Conservative therapy includes taking painkillers, vitamins, anti-inflammatory drugs. The patient goes to physiotherapy, massage, gymnastics. Methods are supplemented by wearing orthopedic devices: plaster casts, special splints, insoles, bandages.
Corrective osteotomy saves time and money. It takes several months after the operation, the patient begins to live fully.
Surgical treatment has a number of contraindications for performance:
- Acute period, severe course of rheumatoid arthritis.
- Active or past infectious diseases (syphilis, bone tuberculosis), their complications.
- Cardiovascular insufficiency stage 3.
- Oncological pathology.
- Respiratory failure of the last stage.
- Confirmed osteoporosis.
- Obesity is a relative contraindication. The operation is performed with the permission of the attending physician.
- Degenerative-dystrophic arthrosis, which is localized in the lateral parts of the joints.
- III stage of patellofemoral arthrosis.
Corrective osteotomy of the foot refers to surgical intervention on the lower extremities. It is carried out in order to restore the physiological functions of the joints.
A procedure such as osteotomy of the knee joint is one of the most sparing forms of surgical intervention in the structure of bone and cartilage tissue. The operation is performed by affecting the tibia or femur in order to reduce pressure on the knee joint. As a rule, it is carried out in the early stages of osteoarthritis and helps to reduce the severity of pain, restore normal mobility of the lower limb.
Indications and contraindications
Basically, corrective osteotomy is used to normalize the motor activity of a patient with deformation and degenerative-dystrophic changes in bone and cartilage tissue. The procedure itself is considered non-traumatic and bloodless, since an incision of no more than one centimeter is made for its implementation.
The main indications for the operation include degenerative changes in the cartilage, which provoke a violation of the axis of the lower limb. This pathological condition occurs due to injuries of soft tissues, ligaments and meniscus. Congenital anomalies of the extremities, the progression of gonarthrosis, and incompletely cured injuries of the knee joint are capable of provoking dystrophic disorders. Osteotomy is performed for disorders that develop against the background of rickets and bone tissue dystrophy.
With special care, osteotomy of the knee joint is performed in the presence of the following pathological conditions:

Preparation for the procedure
Preparatory measures begin with the diagnosis of the patient. The attending physician collects an anamnesis of complaints, a medical history and conducts an external examination of the joint. X-ray and MRI of the affected area are mandatory. Thanks to the data obtained, the orthopedist determines all structural changes in the joint cavity and draws up a plan for restorative measures after surgery. A week before the scheduled procedure, most medications are stopped. Alcohol and smoking are prohibited 14 days prior to knee osteotomy. People with injuries and erosions of the skin are not allowed to operate. In the presence of chronic diseases, it is important to bring them into remission before intervention.
How is it carried out?
Surgical intervention is carried out based on the individual characteristics of the patient's body and the degree of damage to the knee. There is a standard sequence of actions:
 When performing an operation, the doctor takes into account the characteristics of the pathology of a single patient.
When performing an operation, the doctor takes into account the characteristics of the pathology of a single patient. - An incision is made in the skin. After that, their edges are moved apart to the required indicators.
- An artificial graft or a previously prepared part of the patient's femur is inserted into the incision. All parameters are determined by computer calculations.
- A metal plate is placed to hold the bone fragment. For maximum fixation, knitting needles are used.
- The whole procedure is carried out under the control of an x-ray machine. This is necessary for making a fracture in the bone and correct insertion of the plate.
If the surgical intervention is carried out successfully, then the integrity of the patella is completely preserved and the patella tendons are not injured. At the same time, there is a partial restoration of cartilage and a decrease in pain syndrome, by normalizing the process of blood supply and eliminating congestion.